Dealing with unexplained skin issues can be really tough and emotional. Our skin is more than just a shield; it shows our health and happiness. When we get mysterious rashes and symptoms, knowing the difference between psoriasis and shingles is key for good treatment and peace.
Skin rash differences might seem small but are very important. In the U.S., about 7.5 million people have psoriasis, and 1 million get shingles each year. These conditions might look alike at first, but they have different causes, symptoms, and treatments.
This guide will help you understand these skin issues better. It will give you clear insights into their unique traits. Whether you’re dealing with symptoms or just want to know more, learning about these conditions is a big step toward managing them.
Key Takeaways
- Psoriasis and shingles are distinct skin conditions with different causes
- Approximately 1 in 3 individuals will experience shingles in their lifetime
- Accurate diagnosis is critical for effective treatment
- Skin rash differences can be subtle but medically significant
- Both conditions require professional medical evaluation
Understanding Skin Conditions: A Comprehensive Overview
Skin conditions are a big health challenge for millions around the world. We’re diving into the complex world of skin diseases. We’ll look at autoimmune disorders and viral infections that change how our skin looks and feels.
Skin diseases show up in many ways, each with its own traits and effects on health. To really get it, we need to look at it from all angles – medical and personal.
Common Skin Disease Characteristics
Skin conditions are all different, with their own causes and effects. Some key things to know include:
- How common certain skin disorders are
- What genetic and environmental factors trigger them
- The role of inflammation
- Whether they can last a long time
Autoimmune disorders like psoriasis are big challenges. About 2-3% of people worldwide have psoriasis. It shows up as scaly patches on the scalp, elbows, and lower back.
Impact on Quality of Life
The emotional and mental effects of skin conditions are huge. Studies show 70% of people with psoriasis feel it really affects their life. Viral infections like shingles add more stress and pain.
Skin health is more than surface deep – it’s a reflection of our overall well-being.
People with skin conditions often face:
- Feeling down or anxious
- Being judged or stigmatized
- Feeling depressed
- Losing confidence in themselves
We focus on treating the whole person, not just the symptoms. Knowing about autoimmune disorders and viral infections helps patients better understand their health journey.
What Makes Psoriasis and Shingles Different
Psoriasis and shingles are two different skin conditions. They have unique symptoms, causes, and how they progress. Knowing these differences helps patients understand their own skin issues better.
- Psoriasis is a chronic autoimmune disorder with fast skin cell growth
- Shingles is an acute viral infection from the varicella-zoster virus
- Psoriasis affects about 2-3% of the world’s population
- Shingles strikes about 1 in 3 people at some point in their lives
Diagnosing these conditions is different. Psoriasis shows up as thick, scaly patches. Shingles appears as a painful, blistering rash along nerve paths.
“Each skin condition tells a unique story about the body’s internal processes.” – Dermatology Research Institute
| Characteristic | Psoriasis | Shingles |
|---|---|---|
| Nature | Chronic autoimmune condition | Acute viral infection |
| Prevalence | 2-3% of population | 1 in 3 people |
| Primary Symptoms | Thick, scaly skin patches | Painful blistering rash |
| Transmission | Not contagious | Virus can spread |
Our detailed diagnosis criteria highlight the need for a doctor’s evaluation. This is to accurately tell apart these complex skin issues.
The Nature of Psoriasis: An Autoimmune Condition
Psoriasis is a complex autoimmune disorder that changes how skin cells grow and replace themselves. It affects about 125 million people worldwide, making life challenging for those with it.
Research shows that psoriasis disrupts the body’s immune system. Normally, skin cells take 28 days to replace themselves. But for those with psoriasis, this process happens in just a few days, causing skin patches.
Understanding Psoriasis Types
There are several types of psoriasis:
- Plaque psoriasis (most common, representing 80% of cases)
- Guttate psoriasis
- Inverse psoriasis
- Pustular psoriasis
- Erythrodermic psoriasis
Psoriasis Triggers and Risk Factors
Many factors can trigger psoriasis:
- Psychological stress
- Skin injuries
- Heavy alcohol consumption
- Smoking
- Certain medications
*”Psoriasis is not just a skin condition, but a complex autoimmune disorder with far-reaching implications for overall health.”*
About 30% of psoriasis patients may get psoriatic arthritis within 5-10 years. This shows why managing these conditions is so important.
Stress and psoriasis are closely linked. Stress can make symptoms worse, making it hard for patients to cope.
Shingles: A Viral Infection Explained
Shingles is a viral infection caused by the varicella-zoster virus. This virus stays hidden in nerve tissues after someone has had chickenpox. It attacks specific nerves, causing pain and discomfort.
The virus usually comes back in people with weak immune systems, often those over 50. Shingles is known for:
- A painful rash on one side of the body
- Burning or tingling before the rash shows up
- Potential for serious pain and complications
Almost all Americans born before 1980 have had chickenpox. This means they could get shingles later in life. The rash from shingles looks different from other skin problems.
“Shingles is not just a rash, but a neurological experience triggered by a dormant virus,” notes medical experts.
Symptoms of shingles can include:
- Fever
- Headache
- Muscle aches
- Fatigue
Shingles starts with nerve sensitivity and then a rash appears. This rash usually stays on one side of the body. Knowing about shingles helps people spot early signs and get help.
| Characteristic | Description |
|---|---|
| Virus Origin | Varicella-zoster (Chickenpox virus) |
| Primary Age Group | Adults 50 and older |
| Rash Location | Typically one side of body |
| Duration | 7-10 days for active outbreak |
Psoriasis vs Shingles: Key Distinctions
It’s important to know the differences between psoriasis and shingles to get the right treatment. Both affect the skin but in different ways.
Our comparison highlights key differences in how these conditions spread and progress:
Transmission and Contagion
Here’s how they differ in spreading:
- Psoriasis is not contagious and can’t be passed from person to person
- Shingles can spread the varicella-zoster virus to those who haven’t had chickenpox
- About 1 million shingles cases are reported each year in the United States
Duration and Progression
The timeline and nature of these conditions are quite different:
- Psoriasis is a chronic condition with recurring flare-ups
- Shingles usually clears up in 2-4 weeks
- Over 50% of shingles cases happen in people over 60
Knowing these differences helps patients better manage their skin condition.
Our research indicates that psoriasis affects 2-3% of the world’s population. Shingles, on the other hand, impacts about 1 in 3 people at some point in their lives. The unique differences in how they spread, symptoms, and progress show each condition has a distinct impact on health.
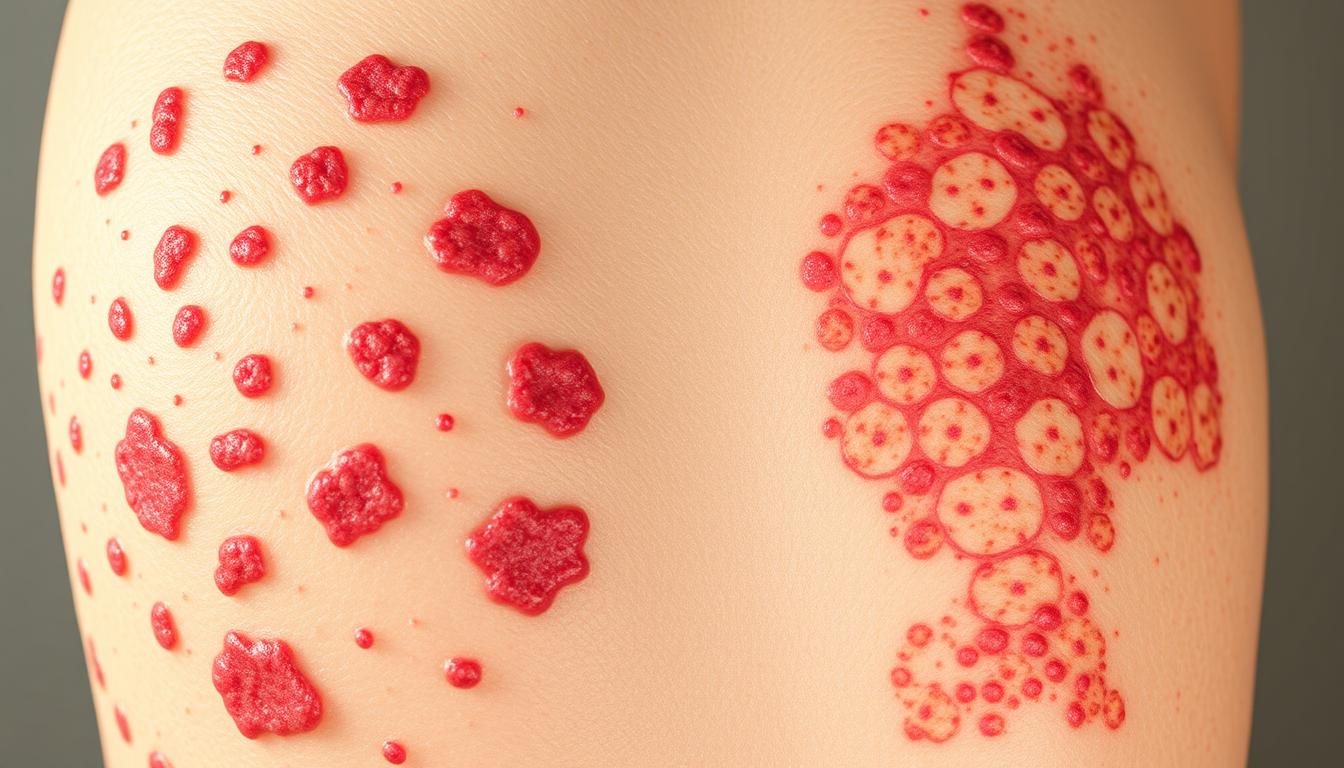
Visual Symptoms and Appearance
It’s important to know the difference between psoriasis and shingles to get the right treatment early. These two conditions look different, making it easier to tell them apart.
Psoriasis has its own signs that make it stand out. 80-90% of psoriasis cases are plaque psoriasis. It shows:
- Red, inflamed patches with silvery-white scales
- Thickened, cracked skin
- Potential nail changes (thickening or crumbling)
- Patches that can appear pink on lighter skin and purple on darker skin tones
Shingles looks very different. Its symptoms show a unique pattern:
- Painful, blistering rash following a specific nerve pathway
- Typically confined to one side of the body
- Rash develops over 3-5 days
- Blisters rupture and form sores within 7-10 days
“The visual appearance of a skin condition can provide critical clues to its underlying cause and severity.” – Dermatology Research Institute
Our comparison shows clear differences in how they look and progress:
| Characteristic | Psoriasis | Shingles |
|---|---|---|
| Color | Red or purple patches | Red with fluid-filled blisters |
| Distribution | Multiple body areas | Localized to one nerve pathway |
| Duration | Chronic, with flare-ups | 2-4 weeks typical rash duration |
Knowing these differences helps people get the right care and understand their skin condition better.
Diagnostic Approaches for Both Conditions
Diagnosing skin issues like psoriasis and shingles needs special medical skills. We use detailed physical checks and advanced tests to find the right treatment.
Doctors use many ways to figure out these tricky skin problems. Patch testing and thorough medical checks are key to finding out what’s causing each problem.
Medical Tests and Examinations
The process includes:
- Looking over the patient’s medical history
- Doing a close-up skin check
- Running special tests like:
- Skin biopsy for psoriasis confirmation
- Viral culture for shingles identification
- Blood tests to check the immune system
Professional Assessment Methods
We look at important things like:
- Looking at symptoms
- Checking if there’s a family history
- Examining the immune system
Getting the right diagnosis is the first step to managing skin issues.
About 3% of U.S. adults have psoriasis, and shingles risks go up after 50. Our methods help patients know their condition and find the best treatments.
Treatment Options for Psoriasis
Psoriasis needs a plan that fits each person. We offer many treatments, from creams to medicines that work all over the body. These help control symptoms and lower skin inflammation.
- How bad the skin lesions are
- How much of the body is affected
- The patient’s overall health
- How well past treatments worked
There are many ways to handle flare-ups. We group treatments into four main types:
- Topical Treatments
- Creams with corticosteroids
- Vitamin D creams
- Salicylic acid products
- Phototherapy
- UVB light therapy
- Targeted light treatments
- Systemic Medications
- Methotrexate
- Cyclosporine
- Oral retinoids
- Biologic Therapies
- TNF-alpha inhibitors
- IL-17 blockers
- IL-23 inhibitors
*”Personalized treatment is key to effectively managing psoriasis symptoms and improving patient quality of life.”*
We focus on care that’s just right for each patient. Every case of psoriasis is different. We aim to treat more than just symptoms. We want to manage the whole condition.
| Treatment Category | Primary Purpose | Typical Duration |
|---|---|---|
| Topical Treatments | Reduce inflammation | Weeks to months |
| Phototherapy | Slow skin cell growth | Months |
| Systemic Medications | Suppress immune response | Months to years |
| Biologics | Target specific immune pathways | Ongoing |
Remember, successful psoriasis management requires patience, consistent treatment, and close collaboration with healthcare professionals.
Managing Shingles: Treatment Protocols
Shingles can be tough and painful. It needs a good treatment plan to manage it well. Knowing the right treatments is key to controlling flare-ups and avoiding long-term problems.
Every year, about 1 million new cases of herpes zoster are found in the United States. This shows how important it is to have good treatment plans.
Antiviral Medications
Antiviral meds are the main treatment for shingles. They help make the outbreak shorter. It’s best to start these meds within 72 hours of the rash showing up.
- Acyclovir
- Valacyclovir
- Famciclovir
Pain Management Strategies
Managing flare-ups also means dealing with pain. This helps lessen discomfort and stops long-term nerve pain.
| Pain Management Approach | Description |
|---|---|
| Over-the-counter Pain Relievers | Acetaminophen and ibuprofen |
| Prescription Pain Medications | Gabapentin or nerve pain specialists |
| Topical Treatments | Lidocaine patches or capsaicin cream |
“Early intervention is key to minimizing the impact of shingles and preventing possible complications.”
Shingles symptoms usually last 3 to 5 weeks. Sometimes, symptoms can last for months. The risk goes up with age, with people over 60 getting about 10 cases per 1,000 each year.
It’s best to talk to a healthcare professional for a treatment plan that fits your needs and medical history.
Prevention Strategies and Vaccines

Managing flare-ups and preventing skin conditions need a full plan. This plan includes medical help and changes in lifestyle. Psoriasis and shingles each have their own challenges for those looking to prevent them.
For those with psoriasis, the goal is to avoid triggers and keep healthy. Important steps include:
- Stress management techniques
- Maintaining a healthy body weight
- Avoiding known skin irritants
- Establishing consistent skincare routines
Shingles prevention focuses on vaccines. Approximately 1 in 3 people will develop shingles in their lifetime. So, preventing it is key.
| Prevention Method | Effectiveness | Recommended Age |
|---|---|---|
| Shingles Vaccine | 90% effective | 50 years and older |
| Psoriasis Lifestyle Changes | Varies by individual | All ages |
“Prevention is always better than cure, specially for chronic skin conditions.”
Our studies show people with psoriasis are 29% more likely to get shingles. This highlights the need for good prevention plans and regular doctor visits.
We suggest talking to doctors to make a prevention plan that fits your health and risks.
Long-term Health Implications
Understanding chronic and acute conditions is key. Skin disorders like psoriasis and shingles affect more than just the skin. They have deep health impacts.
Understanding Chronic and Acute Conditions
Psoriasis is a chronic condition that needs constant care. It’s different from shingles, which is an acute condition. Studies show that 80% of psoriasis patients have plaque psoriasis, affecting their life quality.
- Chronic psoriasis increases cardiovascular disease risks
- Potential for developing comorbidities
- Psychological impacts on mental health
Quality of Life Impact
The World Health Organization points out the big psychological burden of chronic skin conditions. People with psoriasis face higher risks of:
- Depression
- Social isolation
- Reduced work productivity
“Skin conditions are more than physical—they’re deeply personal experiences that affect every aspect of life.”
Shingles, usually an acute condition, can cause long-term pain. The chance of getting shingles is between 10% and 20% for most people. This shows why it’s important to know about these health issues.
Getting professional medical help is vital for managing both chronic and acute skin conditions. It helps patients stay healthy and improve their quality of life.
When to Seek Medical Attention
Knowing when to see a doctor for psoriasis or shingles is key to your health. Our experts say to watch for certain signs. These signs mean you need to see a doctor right away.
Here are the main signs to look out for:
- Persistent rash spreading across multiple body areas
- Intense pain or burning sensations
- Signs of possible infection
- Rash near eyes or affecting vision
- Fever with skin symptoms
Dermatologists stress the need for early action. Early treatment can greatly reduce complications. People over 50 are at higher risk, with 1 in 3 getting shingles.
“Early detection and treatment are key to managing skin conditions well” – Dermatology Research Institute
See a doctor right away if you notice:
- Unusual skin changes lasting more than a week
- Severe pain with skin eruptions
- Symptoms that affect your daily life
- Family history of autoimmune skin conditions
Call TK Dermatology at (352) 565-7575 for expert care. Our team is ready to help with quick diagnosis and treatment.
The Role of Dermatologists in Treatment
Dermatologists are key healthcare experts who focus on treating complex skin issues like psoriasis and shingles. They do more than just look at your skin. They provide detailed care that tackles both immediate and long-term needs.
Dermatologists offer a variety of treatments based on what each patient needs. For conditions like psoriasis and shingles, they use advanced tests to create specific plans. They know the differences between skin problems, ensuring the right treatment.
- Comprehensive skin examinations
- Advanced diagnostic techniques
- Personalized treatment protocols
- Ongoing symptom management
Our dermatology team knows that everyone’s skin issues are different. They use the latest tools to check symptoms, figure out the exact condition, and make treatment plans just for you. Getting the right diagnosis is key to managing skin diseases well.
“Expertise in dermatology means understanding the intricacies of skin health and providing caring, focused care.” – Skin Health Professionals Association
Patients get the best care from dermatologists’ deep knowledge of treatments. For shingles, this could mean antiviral meds and ways to manage pain. For psoriasis, treatments might include creams or even biologic therapies.
| Condition | Diagnostic Focus | Treatment Approach |
|---|---|---|
| Psoriasis | Skin lesion evaluation | Personalized medication plan |
| Shingles | Viral infection assessment | Antiviral and pain management |
We know how important dermatologists are in changing lives. They offer top-notch care, helping people manage chronic skin issues. This reduces symptoms and boosts their quality of life.
Living with Psoriasis and Shingles
Managing chronic conditions like psoriasis and shingles needs a full plan. This plan tackles both physical and emotional hurdles. Our goal is to empower patients to handle these health challenges well.
People with psoriasis or recovering from shingles face big daily challenges. It’s key to know how to manage flare-ups and keep a good quality of life.
- Develop consistent treatment routines
- Practice stress management techniques
- Connect with support networks
- Monitor symptoms closely
“Knowledge and preparation are your best allies in managing chronic skin conditions.”
For those with psoriasis, managing flare-ups is a multi-step process. Making lifestyle changes, reducing stress, and using specific medical treatments can help a lot.
| Condition | Prevalence | Key Management Strategy |
|---|---|---|
| Psoriasis | 7.5 million Americans | Regular dermatologist consultations |
| Shingles | 1 million cases annually | Early medical intervention |
Vaccination is key in prevention. The CDC suggests Shingrix for those 50 and older, and even more for those with chronic conditions. Proactive healthcare decisions can greatly lower risks of complications.
Emotional support is just as vital. Joining support groups, getting counseling, and talking openly with doctors helps patients deal with these chronic conditions.
Latest Research and Medical Advances
The field of dermatology is growing fast, with new treatments for psoriasis and shingles. We’re seeing big steps forward in how we treat these conditions. These advances aim to make treatments more precise and effective.

Current Cutting-Edge Studies
Recent studies have shown promising ways to treat skin problems. Some highlights include:
- FDA approval of Bimekizumab (Bimzelx) in October 2023 for moderate to severe plaque psoriasis
- New biologics targeting specific immune pathways
- Advanced JAK inhibitors showing significant promise for psoriasis management
Future Treatment Possibilities
New technologies are changing how we see autoimmune diseases. Researchers are looking into new treatments that could change patient care:
- Personalized genetic therapies
- More precise biologic interventions
- Oral medications replacing injectable treatments
The future of dermatological treatment lies in understanding individual genetic markers and developing targeted, patient-specific therapies.
Studies on JAK inhibitors like tofacitinib and baricitinib are showing great promise. These drugs might offer a pill option instead of injections. This could make treatment easier for patients and improve their lives.
We’re dedicated to turning these research findings into real treatments for patients with complex skin issues.
Conclusion
We’ve looked into psoriasis and shingles, two different skin issues. Both can cause skin rashes, but they come from different sources. Psoriasis is an autoimmune disease, while shingles is caused by a virus.
Research shows that psoriasis affects 0.91% to 8.5% of adults. It has big health implications. There’s a link between psoriasis and shingles, with some people at higher risk, like those aged 20-39.
Knowing about these conditions takes a lot of medical knowledge. It’s important to get help from a dermatologist. They can give the right treatment and advice.
If you need help with psoriasis or shingles, call TK Dermatology at (352) 565-7575. Our team is ready to help you take care of your skin.