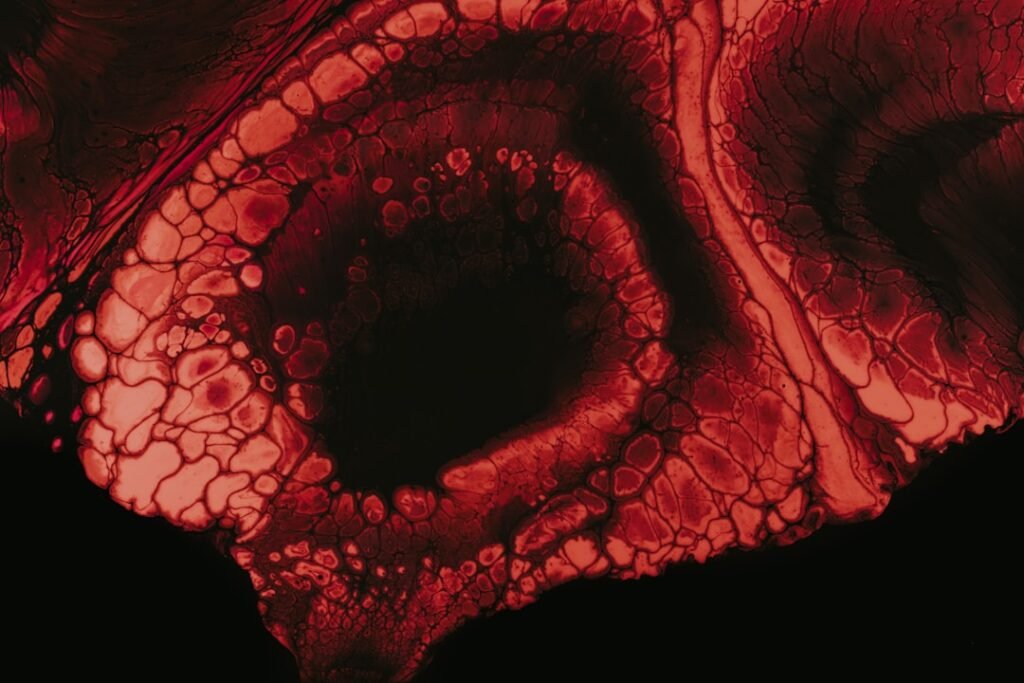
Post Inflammatory Erythema (PIE) is a skin condition characterized by the presence of red or pink marks that appear on the skin following an inflammatory event. This phenomenon is particularly common in individuals with darker skin tones, where the contrast between the affected area and the surrounding skin can be more pronounced. PIE is often mistaken for post-inflammatory hyperpigmentation (PIH), but the two conditions are distinct; while PIH involves darkening of the skin, PIE manifests as redness.
The redness is a result of increased blood flow to the area as part of the body’s healing response, and it can persist for weeks or even months after the initial inflammation has resolved. The inflammatory events that lead to PIE can vary widely, including acne lesions, eczema flare-ups, allergic reactions, or even minor injuries. The condition is not limited to any specific age group or demographic, although it is frequently observed in individuals with acne-prone skin.
Understanding PIE is crucial for effective management and treatment, as it can significantly affect an individual’s self-esteem and overall quality of life. The redness associated with PIE can be particularly distressing for those who are already dealing with the underlying skin issues that caused the inflammation in the first place.
Key Takeaways
- Post Inflammatory Erythema (PIE) is a type of skin discoloration that occurs after an inflammatory acne breakout or injury to the skin.
- Causes of PIE include acne, eczema, psoriasis, and other skin conditions, as well as trauma to the skin from burns or cuts.
- Symptoms of PIE include red or pink marks on the skin that do not fade, even after the original inflammation has healed.
- Diagnosis of PIE is usually based on the appearance of the skin, and treatment options may include topical creams, laser therapy, or chemical peels.
- Preventing PIE involves treating and preventing the underlying skin conditions, avoiding picking or squeezing acne, and using sunscreen to protect the skin from further damage.
Causes of Post Inflammatory Erythema
The primary cause of post-inflammatory erythema is the body’s natural inflammatory response to injury or irritation. When the skin experiences trauma—whether from acne, dermatitis, or other inflammatory conditions—blood vessels in the affected area dilate to facilitate healing. This increased blood flow results in the characteristic redness associated with PIE.
Factors such as skin type, genetics, and the severity of the initial inflammation can influence how pronounced this redness becomes and how long it lasts. Acne is one of the most common triggers for PIE. When acne lesions form, they can cause significant inflammation in the surrounding skin.
Once the acne resolves, the residual redness may linger long after the blemish has healed. Other conditions that can lead to PIE include rosacea, psoriasis, and even certain cosmetic procedures like chemical peels or laser treatments. Additionally, external factors such as sun exposure can exacerbate PIE by increasing blood flow to already inflamed areas, making it essential for individuals prone to this condition to adopt protective measures against UV radiation.
Symptoms and Characteristics of Post Inflammatory Erythema
The hallmark symptom of post-inflammatory erythema is the presence of red or pink patches on the skin that appear after an inflammatory event. These patches can vary in size and intensity, often resembling a sunburn or a rash. Unlike post-inflammatory hyperpigmentation, which presents as dark spots, PIE is characterized by its bright red hue, which may fade over time but can take several weeks to months to fully resolve.
The affected areas may feel warm to the touch due to increased blood flow and may be accompanied by mild itching or tenderness.
In terms of distribution, PIE commonly occurs on the face, particularly on the cheeks and forehead, but it can also appear on other parts of the body where inflammation has occurred. The duration of PIE can vary significantly from person to person; some individuals may notice improvement within a few weeks, while others may experience persistent redness for several months. The condition does not typically cause pain or discomfort beyond mild irritation, but its visible nature can lead to emotional distress for those affected.
Diagnosis and Treatment Options
| Diagnosis and Treatment Options | |
|---|---|
| Diagnostic Test | Treatment Option |
| Blood Test | Medication |
| Imaging (X-ray, MRI, CT scan) | Surgery |
| Biopsy | Radiation Therapy |
Diagnosing post-inflammatory erythema typically involves a thorough clinical evaluation by a dermatologist. The physician will assess the patient’s medical history, examine the affected areas, and rule out other skin conditions that may present similarly. In many cases, a diagnosis can be made based on visual inspection alone; however, if there is uncertainty, a biopsy may be performed to confirm that there are no underlying issues contributing to the symptoms.
Treatment options for PIE focus primarily on reducing inflammation and promoting healing. Topical treatments such as corticosteroids may be prescribed to alleviate redness and swelling. Additionally, products containing niacinamide or azelaic acid can help improve skin tone and reduce redness over time.
For more severe cases or persistent PIE, dermatologists may recommend laser therapy or intense pulsed light (IPL) treatments, which target blood vessels in the skin to reduce redness effectively. These procedures can provide significant improvement in appearance but may require multiple sessions for optimal results.
How to Prevent Post Inflammatory Erythema
Preventing post-inflammatory erythema involves a multifaceted approach aimed at minimizing skin irritation and inflammation. One of the most effective strategies is to manage underlying skin conditions proactively. For individuals prone to acne or eczema, adhering to a consistent skincare routine that includes gentle cleansing and moisturizing can help reduce flare-ups that lead to PIE.
It is also essential to avoid picking at blemishes or inflamed areas, as this can exacerbate inflammation and increase the risk of developing PIE. Sun protection plays a critical role in prevention as well. Ultraviolet (UV) rays can worsen existing redness and prolong healing time.
Using broad-spectrum sunscreen with an SPF of 30 or higher daily is crucial for anyone at risk of PIE. Additionally, wearing protective clothing and seeking shade during peak sun hours can further shield sensitive skin from harmful UV exposure. Incorporating anti-inflammatory ingredients into skincare products—such as green tea extract or chamomile—can also help soothe irritated skin and reduce the likelihood of developing PIE after an inflammatory event.
Differentiating post-inflammatory erythema from other skin conditions is essential for appropriate treatment and management. One common condition that often gets confused with PIE is post-inflammatory hyperpigmentation (PIH). While both conditions occur following an inflammatory event, they differ significantly in appearance; PIH presents as dark brown or black spots on the skin due to excess melanin production, whereas PIE is characterized by red or pink patches resulting from increased blood flow.
Another condition that may be mistaken for PIE is rosacea, which also causes facial redness but typically includes additional symptoms such as flushing, visible blood vessels, and sometimes acne-like bumps. Unlike PIE, rosacea is a chronic condition that requires ongoing management rather than being a temporary response to inflammation. Understanding these distinctions is vital for individuals seeking treatment options; misdiagnosis can lead to ineffective treatments and prolonged distress.
The Emotional Impact of Post Inflammatory Erythema
The emotional impact of post-inflammatory erythema can be profound, particularly for those who are already struggling with underlying skin issues like acne or eczema. The visible nature of PIE often leads to feelings of self-consciousness and embarrassment, which can affect social interactions and overall quality of life. Many individuals report feeling anxious about their appearance, leading them to avoid situations where they might be exposed to scrutiny or judgment.
Moreover, the persistence of redness associated with PIE can contribute to a cycle of frustration and low self-esteem. As individuals seek solutions to manage their skin condition, they may encounter various treatments that promise results but fail to deliver immediate relief. This experience can lead to feelings of hopelessness and exacerbate mental health issues such as anxiety or depression.
It is essential for those affected by PIE to seek support from healthcare professionals who understand the emotional toll of skin conditions and can provide both medical treatment and psychological support.
Living with Post Inflammatory Erythema: Coping Strategies and Support
Living with post-inflammatory erythema requires a combination of effective coping strategies and support systems. One practical approach is to establish a skincare routine tailored to sensitive skin that minimizes irritation while promoting healing.
This routine should include gentle cleansers, non-comedogenic moisturizers, and targeted treatments for redness reduction.
Keeping a consistent regimen helps individuals feel more in control of their skin health. Support from friends, family, or online communities can also play a crucial role in coping with the emotional challenges posed by PIE. Sharing experiences with others who understand what one is going through can provide comfort and validation.
Many find solace in connecting with support groups or forums dedicated to skincare issues where they can exchange tips and encouragement. Additionally, mindfulness practices such as meditation or yoga can help manage stress levels associated with living with a visible skin condition. These practices promote relaxation and self-acceptance, which are vital for maintaining mental well-being amidst physical challenges.
By combining effective skincare strategies with emotional support and self-care practices, individuals living with post-inflammatory erythema can navigate their journey toward healthier skin with greater resilience and confidence.
If you are interested in learning more about skin conditions and treatments, you may want to check out this article on using fat injections to lose weight. This article discusses the procedure, benefits, and risks associated with using fat injections for weight loss. It is important to stay informed about different treatment options and their potential outcomes when dealing with skin issues like post inflammatory erythema.
FAQs
What is post inflammatory erythema?
Post inflammatory erythema (PIE) is a type of skin discoloration that occurs after an inflammatory acne lesion has healed. It appears as red or pink marks on the skin and is caused by the dilation of blood vessels in the affected area.
What causes post inflammatory erythema?
Post inflammatory erythema is caused by the body’s inflammatory response to acne lesions. When the skin is inflamed, the blood vessels in the affected area dilate, leading to the red or pink discoloration that characterizes PIE.
How is post inflammatory erythema treated?
Treatment for post inflammatory erythema may include topical treatments such as retinoids, azelaic acid, or niacinamide, as well as laser or light therapies. It is important to consult a dermatologist for a personalized treatment plan.
Is post inflammatory erythema permanent?
Post inflammatory erythema is not permanent and typically fades over time. However, it may take several months to years for the discoloration to completely resolve. Proper treatment and skincare can help speed up the fading process.
Can post inflammatory erythema be prevented?
Preventing post inflammatory erythema involves treating acne lesions promptly to minimize inflammation and avoiding picking or squeezing acne, which can worsen inflammation and increase the risk of PIE. Using sunscreen and gentle skincare products can also help prevent exacerbation of PIE.