Did you know that up to 40% of adults face skin barrier issues at some point? Your skin works hard to protect you, but you might not realize it’s failing until you see symptoms.
Maybe you’ve woken up with dry skin or felt your skin feel tight and uncomfortable. These small changes can mean big things are happening under the surface. Your skin’s outer layer, the first defense, might be weakened.
This article will show you common signs that your skin barrier needs help. You’ll see what these signs look like and why they happen.
Important note: The info here is for learning, not for diagnosing or replacing doctor visits. Everyone’s skin reacts differently to the world around them, their habits, and aging. If you’re worried about your skin, see a dermatologist for the right advice and care.
We’ll talk about spotting early signs, what causes damage, and when to get expert help. Knowing these basics helps you take better care of your skin.
Key Takeaways
- Your skin’s protective barrier can become compromised due to weather, lifestyle choices, and skincare habits
- Early warning signals include unexpected dryness, tightness, and increased sensitivity to products
- Up to 40% of adults experience barrier dysfunction at some point in their lives
- This article provides educational information, not medical diagnosis or treatment advice
- Consulting a board-certified dermatologist is essential for persistent or severe symptoms
- Recognizing early changes helps you take proactive steps toward healthier skin
Understanding the Skin Barrier Function
Your skin’s barrier is always working to protect you. It keeps your body safe from the outside world. Knowing how it works helps you spot problems early.
Skin changes can happen for many reasons. This includes weather changes and reactions to products. Understanding your skin barrier helps you act fast to protect it.
The Structure and Composition of Your Protective Layer
The skin barrier is called the stratum corneum. It’s the outermost layer of your skin. It’s made of dead skin cells called corneocytes that protect you.
Think of your skin barrier like a brick wall. The corneocytes are the bricks, and lipids are the mortar. These lipids include ceramides, cholesterol, and fatty acids that hold the cells together.
Your barrier also has a protein called filaggrin. It helps create natural moisturizing factors (NMF). These keep your skin hydrated. When barrier lipid depletion happens, your protection weakens.
Why Barrier Health Matters for Your Skin
A healthy skin barrier is key to your skin’s health. It prevents moisture loss, keeping your skin plump and smooth. This makes your skin look and feel good.
Your barrier also keeps your skin’s pH level right. This is slightly acidic, which stops bad bacteria and helps good ones. If your barrier weakens, this balance can shift, leading to problems.
A strong barrier makes your skin look better and feel more comfortable. Moisture barrier damage can make your skin dull and rough. It also makes your skin age faster and harder to heal.
A weak barrier makes your skin more sensitive. Even gentle products can cause reactions. This makes it hard to find products that work without irritating your skin.
Defense Mechanisms That Keep You Safe
Your skin barrier protects you from many dangers every day. It blocks UV rays and keeps out pollutants and extreme weather. This protects your deeper skin layers.
It also stops harmful microorganisms from getting in. The tight connections between cells make it hard for bacteria, viruses, and fungi to enter. This keeps you safe from infections.
The barrier controls moisture and keeps out unwanted substances. It lets good things in but keeps bad ones out. This keeps your skin healthy and stable.
Your barrier works hard to keep your skin healthy. It adjusts to challenges and keeps your skin balanced. When it’s working right, you might not even notice it.
Knowing how your barrier works shows why it’s so important. Any signs of trouble mean it needs help. Catching these early can prevent bigger problems.
Common Signs of Skin Barrier Breakdown
Spotting signs of skin barrier breakdown means paying attention to how your skin looks and feels. It shows distress through visible and physical changes. These signs often start slowly, making them easy to overlook.
Knowing these signs helps you see when your skin needs extra care. Here are the most common signs that your barrier might be damaged.
Dryness and Flakiness
Dryness is a clear sign of a damaged skin barrier. When the barrier can’t hold moisture, your skin feels tight and dry. This is different from the dryness you feel when it’s cold outside.
A damaged barrier lets water escape, causing dryness. Your skin’s natural moisturizers can’t work right without the lipid layer. You might notice your skin feels rough and doesn’t get better with moisturizer.
Flakiness happens when dead skin cells don’t fall off right. Without enough lipids, they stick together, causing flakes. Affected areas look dull and lackluster, unlike healthy skin.
This problem doesn’t go away with just water. You might use moisturizer many times a day, but your skin stays dry. It can also get rough patches, like on your cheeks or nose.
Redness and Irritation
A weak barrier lets irritants in, causing inflammation. This shows as redness, blotchiness, or visible blood vessels. Redness can be in patches or cover more of your face.
You might feel warmth and see inflammation in these areas. Your skin can look flushed or reddish, even without heat or exercise. This redness doesn’t go away fast, unlike a temporary flush.
Some people get irritation in areas exposed to stressors. Without a strong barrier, the skin can’t fight off pollution or harsh cleaners. This leads to ongoing inflammation.
This inflammation can feel uncomfortable, from warmth to burning. You might see bumps, uneven texture, or inflamed areas. These signs mean your skin is trying hard to protect itself but can’t.
Increased Sensitivity to Products
One key sign is sudden reactions to products that used to be okay. A weak barrier lets products penetrate too deeply or let irritants through. You might feel stinging or burning when using familiar products.
This heightened skin sensitivity can affect more than skincare. Even water that used to feel fine now feels too hot. Fabrics or wind can also cause discomfort.
The barrier lets active ingredients reach deeper than they should. Even gentle products can cause reactions because the barrier isn’t filtering properly. You might find you can’t use products with fragrances or certain preservatives.
This sensitivity can start slowly or suddenly, after stress, illness, or environmental changes. Products with acids, retinoids, or vitamin C might now cause discomfort. Your skin becomes hyper-reactive to things it used to handle well.
| Symptom Category | Normal Skin Response | Compromised Barrier Response | Duration |
|---|---|---|---|
| Moisture Retention | Stays hydrated between moisturizer applications | Feels tight and dry within hours of moisturizing | Persistent, ongoing |
| Texture Quality | Smooth, soft, even surface | Rough patches, visible flakes, uneven areas | Continues for weeks |
| Visual Appearance | Even tone, minimal redness | Blotchy, red patches, visible inflammation | Doesn’t resolve quickly |
| Product Tolerance | Comfortable application, no stinging | Burning, tingling, immediate discomfort | Occurs with multiple products |
| Overall Feel | Comfortable, resilient, balanced | Tender, reactive, sensitive to touch | Affects daily comfort |
Other signs include loss of elasticity and fine lines becoming more noticeable. A weak barrier can’t keep the skin hydrated, leading to these issues. Increased acne or breakouts can also happen because bacteria can get in more easily.
The skin may show signs of infections more often. A healthy barrier keeps out bacteria and viruses, but a weak one can’t. This can lead to uneven pigmentation or dark spots as the skin tries to repair itself.
These signs often happen together. You might see dryness and sensitivity at the same time, or redness with flakiness. Recognizing these patterns helps you know when your skin needs extra help to stay healthy.
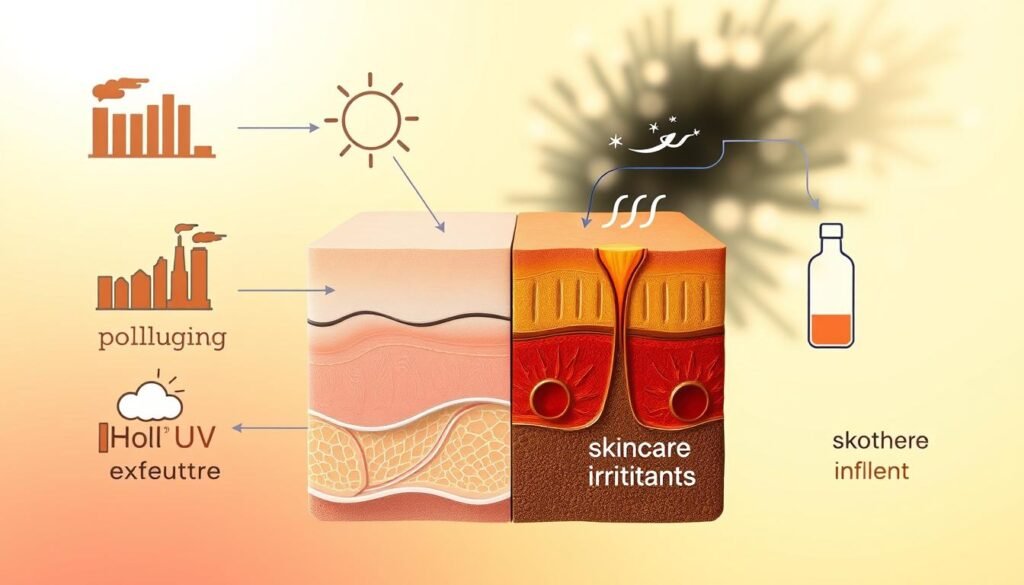
Factors Contributing to Skin Barrier Damage
Many things in your world and daily life quietly harm your skin’s shield. Knowing what these are helps you make better choices. Some things you can’t change, but knowing them lets you protect yourself and seek compromised skin barrier treatment when needed.
External Conditions That Weaken Protection
Your surroundings greatly affect your skin’s strength. The air, climate, and toxins you face all play a part in how well your skin works.
Extreme weather is tough on your skin. Cold and dry air takes moisture away, while hot weather messes with your skin’s pH.
Air pollution is a big problem. It causes stress that harms your skin cells. Pollutants from cars and factories settle on your skin, causing inflammation and weakening your barrier.
- UV radiation: Damages collagen and elastin, breaking down your skin’s structure
- Low humidity environments: Cause your skin to lose water, making it dry and weak
- Allergens and irritants: Cause your immune system to react, leading to skin barrier inflammation and weakened defenses
- Seasonal changes: Make your skin work hard to adapt, sometimes too hard
- Indoor heating and cooling: Dry out the air, stressing your skin barrier
You can’t control everything, but knowing these factors helps you protect yourself. Simple steps like using a humidifier or applying antioxidant serums can help fight environmental damage.
Daily Habits That Impact Barrier Strength
Your lifestyle choices deeply affect your skin’s health. Sleep, diet, and stress levels all impact your skin’s barrier.
Not getting enough sleep hurts your skin’s repair process. Your skin heals best between 10 PM and 2 AM.
Stress raises cortisol levels, causing inflammation and weakening your barrier. This might require compromised skin barrier treatment.
- Smoking: Reduces blood flow and oxygen to skin cells, hindering repair
- Poor nutrition: Lacks essential fatty acids, vitamins, and minerals for barrier health
- Insufficient hydration: Limits moisture and supports cellular functions
- Alcohol consumption: Depletes water and disrupts lipid composition
- Physical stress: Diverts resources from skin repair
These factors work together. Someone who smokes, drinks a lot, and doesn’t sleep well faces a lot of barrier damage.
But, making positive changes can help a lot. Better sleep and more water can strengthen your barrier in weeks.
Common Skincare Mistakes
Good intentions can sometimes harm your skin. Many people unknowingly strip away their skin’s natural protection while trying to improve it.
Washing your face too much is a big mistake. It removes beneficial oils, causing skin barrier inflammation and weakening your skin.
Water temperature is important. Hot showers and face washing melt away the lipid layer, leaving your skin exposed.
- Harsh exfoliation: Creates tears in the skin surface
- High pH cleansers: Disrupts the acid mantle that protects against harmful bacteria
- Applying actives without moisturizer: Allows ingredients to penetrate too deeply, causing irritation
- Frequent product changes: Prevents skin adaptation and introduces incompatible ingredients
- Skipping sunscreen: Exposes your barrier to UV damage
- Using too many products: Overwhelms skin with conflicting ingredients
Each of these practices harms your barrier in different ways. Knowing why they cause problems helps you avoid them.
To fix this, simplify your routine and choose gentler products. Use lukewarm water, pH-balanced cleansers, and moisturize well to protect your barrier while keeping your skin clean and healthy.
Seasonal Changes and Your Skin Barrier
Seasonal changes bring different stressors that affect your skin’s barrier. Knowing how weather impacts your skin helps you stay ahead. Each season has unique challenges that need specific care.
Your skin interacts with the world around it. Temperature, humidity, and allergens all affect your barrier. By understanding these patterns, you can prepare your skincare routine.
Cold Weather Challenges
Winter is tough on your skin’s barrier. Cold air and low humidity cause transepidermal water loss. This pulls moisture from deeper layers to the surface, where it evaporates fast.
Heating systems make indoor air dry. This dry air, with humidity below 20 percent, is bad for your skin. It makes moisture loss worse.
Cold wind also stresses your skin. Wind can damage the outer skin layer. Plus, your body makes less sebum in winter, which helps keep moisture in.
Many people get “winter skin” even if they’re not usually dry. It feels tight, flaky, and itchy. The cold weather and dry air overwhelm even strong skin barriers.
Warm Weather Risks
Summer poses its own challenges, with UV rays being a big one. UV rays damage collagen and elastin, and harm the lipids that keep skin cells together. This leads to skin barrier dysfunction that builds up over time.
Sunburn is a clear sign of barrier damage. It causes inflammation, peeling, and sensitivity. Even without visible burns, UV rays damage your skin at a molecular level.
Summer heat makes you sweat more. This can upset your skin’s pH balance. Chlorinated pools and salt water also strip away protective oils, making your skin more vulnerable.
People often wash their skin too much in summer. This removes beneficial lipids faster than they can be replaced. This weakens your barrier, even with more washing.
Allergy Season Effects
Seasonal allergies can harm your skin barrier. When your immune system reacts to allergens, it causes inflammation. This weakens your barrier, even in areas not directly exposed.
Allergies can also physically damage your skin. Nose-blowing, eye-rubbing, and tissue use wear down your skin’s barrier. This makes the skin around your nose and eyes red, raw, and sensitive.
Allergy meds help symptoms but can dry out your skin. Antihistamines can lower moisture levels in your body, including your skin. This adds stress to your barrier during allergy seasons.
Knowing these seasonal patterns helps you prepare your skincare routine. By strengthening your barrier before seasonal stressors, you can reduce the impact of skin changes.
The Role of Aging in Skin Barrier Health
As we age, our skin barrier changes in ways that affect its protection and moisture retention. These changes are natural and not a sign of neglect. Knowing how aging affects our skin helps us adjust our skincare routine.
Aging and skin health are closely linked. Factors like cell regeneration and hormonal changes play a big role. Understanding these changes helps us spot normal aging versus issues that need attention.
Natural Aging Process
Our skin barrier regenerates all the time, but it slows down with age. Younger skin can repair itself in about six to seven hours after damage. But, as we get older, this process takes much longer.
This slower repair means damaged skin barrier symptoms last longer and need more care. The outer layer of our skin, the stratum corneum, gets less efficient at replacing dead cells with new ones.
- Cell turnover rate decreases, leading to slower healing and recovery
- Natural moisturizing factor production diminishes, reducing hydration capacity
- Ceramide content drops significantly, weakening lipid structure
- Collagen and elastin synthesis declines, affecting structural support
- Barrier thickness may decrease, increasing vulnerability to environmental stressors
Barrier lipid depletion is a big change with age. The lipid matrix that holds skin cells together loses density and organization. This creates gaps that let more water escape.
Collagen and elastin do more than just make skin look young. They help keep the barrier strong. As these proteins decrease, our skin becomes less able to handle outside challenges.
Hormonal Changes Over Time
Hormonal shifts throughout life affect our skin barrier. These changes impact skin function in many ways, from oil production to how it reacts to inflammation. Knowing this helps explain why skin can become more sensitive at certain times.
Menopause is a big change for skin barrier health. The drop in estrogen affects how well skin holds moisture, its thickness, and lipid production. Many women find their skin dries out and becomes more sensitive during this time.
Sebum production changes with hormone shifts, leading to drier skin in older age. This means the skin barrier gets less natural protection. It also changes how it responds to inflammation and heals from minor damage.
Hormonal shifts are ongoing, not just one-time events. Androgens, thyroid hormones, and growth factors all impact barrier health. The combined effect creates a complex situation where many factors interact at once.
Preventative Measures for Aging Skin
While aging is inevitable, you can slow down barrier decline with the right choices. Proactive steps help keep your barrier healthy at any age. The key is knowing what mature skin needs most.
Gentle cleansing practices become more important as skin ages. Harsh cleansers can strip away essential lipids from older skin. Choose mild, pH-balanced cleansers that remove impurities without harming protective oils.
Using products that support the barrier makes a big difference. Ingredients like ceramides, fatty acids, and cholesterol help replace lost lipids. These ingredients are similar to the natural substances that decrease with age.
Here are some preventative measures to consider:
- Apply broad-spectrum sunscreen daily to prevent additional photodamage
- Use rich moisturizers that seal in hydration and support lipid composition
- Avoid over-exfoliation, which can compromise already slower-regenerating barriers
- Consider targeted treatments with niacinamide or peptides that support barrier function
- Maintain consistent hydration through both topical products and water intake
Lifestyle choices also help protect your skin. Getting enough sleep supports cell repair. Eating a balanced diet rich in omega-3s and antioxidants helps maintain barrier health. Managing stress also helps keep inflammation in check.
The way we address damaged skin barrier symptoms should change as we age. What worked in your 30s may not be enough in your 60s. Regularly updating your skincare routine ensures it continues to support your skin’s health at every stage of life.
Identifying Temporary vs. Chronic Issues
When your skin barrier shows trouble, knowing if it’s temporary or chronic is key. Some issues clear up in days or weeks. Others might show deeper problems that need doctor’s care. Spotting these patterns helps you act fast and avoid worry or late treatment.

Telling apart temporary reactions and chronic conditions can be tricky. But, watching your symptoms over time and their context can give clues about your skin.
Recognizing Short-Term Versus Long-Term Effects
Temporary barrier issues usually come from clear causes. You might see changes after hot showers, harsh winds, or new products. These issues often start with a specific event or change.
Temporary skin barrier problems share several common characteristics:
- They appear shortly after a specific trigger or environmental exposure
- Symptoms remain localized to areas that contacted the irritant
- Your skin begins improving within 3-7 days once you remove the trigger
- Basic barrier repair strategies like gentle cleansing and moisturizing provide relief
- The issue doesn’t recur unless you encounter the same trigger again
For example, if your skin gets dry and sensitive from a new product, stopping it and using gentle products should help in a week or two. This shows it’s a temporary issue.
Chronic or recurring issues are different. They last long, even with good skincare and avoiding irritants. Your skin might not fully recover between flare-ups, or symptoms keep coming back without clear reasons.
Patterns that suggest more persistent barrier concerns include:
- Symptoms lasting beyond four weeks despite appropriate home care
- Recurring episodes that happen without obvious external causes
- Progressive worsening over months instead of getting better
- Symptoms that significantly impact your sleep, comfort, or daily activities
- Skin changes accompanied by other symptoms like joint pain or fatigue
Medical conditions like adult acne, atopic dermatitis, ichthyosis, rosacea, and psoriasis can affect the skin barrier. Dermatitis from barrier damage can come from outside factors or these conditions. Getting a professional check-up is key when symptoms don’t go away.
| Characteristic | Temporary Issues | Chronic Conditions |
|---|---|---|
| Onset | Sudden, after identifiable trigger | Gradual or recurring without clear cause |
| Duration | Days to 2-3 weeks | Beyond 4 weeks or recurring cycles |
| Response to Care | Improves with basic barrier repair | Limited improvement despite consistent care |
| Pattern | Single episode with resolution | Persistent or repeatedly returning symptoms |
Knowing When Professional Guidance Matters
Seeing a dermatologist doesn’t mean you’ve failed at skincare. It’s a smart choice to get help and treatments you can’t find over the counter. Dermatologists can find underlying issues, prescribe treatments, and prevent complications from untreated barrier problems.
Consider scheduling a dermatology consultation when you notice:
- Symptoms persisting beyond three to four weeks despite gentle skincare practices
- Sudden onset of severe dryness, redness, or sensitivity without obvious cause
- Signs suggesting infection, such as oozing, honey-colored crusting, or fever
- Painful cracks or fissures that don’t heal with moisturization
- Barrier issues that wake you at night due to itching or discomfort
- Uncertainty about whether your current routine helps or worsens your condition
Early treatment often prevents bigger problems. A dermatologist can tell if your symptoms are simple irritation, contact dermatitis, or need compromised skin barrier treatment with prescription meds. They can also figure out if environmental changes, diet, or health issues affect your skin.
Professional help is key when you’ve tried many products without seeing improvement. Sometimes, what looks like ongoing barrier damage is actually sensitivity to common skincare ingredients. A dermatologist can do patch tests to find out what’s causing the problem and suggest the right products for you.
You might also need professional advice if you’re dealing with more than one skin issue at once. Conditions like rosacea or skin and scalp health issues need a treatment plan that covers barrier function and other symptoms. A full check-up ensures you’re treating the right problem without making another worse.
It’s normal for your skin to take time to respond to the right care, even if barrier damage has been going on for months. But, you should see your skin start to get better, not worse. If your condition doesn’t improve or gets worse despite following your dermatologist’s advice, tell them so they can adjust your treatment.
Effective Strategies for Strengthening the Skin Barrier
Recognizing moisture barrier damage is the first step. Taking action to repair it is key. Focus on practices that help your skin retain moisture and protect against stress.
Repairing your skin barrier involves hydration, choosing the right ingredients, and avoiding harmful substances. These steps help rebuild the lipid layer that keeps your skin healthy.
Supporting Moisture Retention Daily
Hydration and moisturization are different. Hydration adds water to your skin cells. Moisturization seals in that moisture and provides essential lipids.
Water temperature is important. Hot water can melt away your skin’s natural oils. Use lukewarm water when washing your face to keep those oils.
Apply moisturizer within three minutes of washing while your skin is damp. This helps trap water in your skin.
Layering products is key. Start with thinner formulas and move to thicker ones. This ensures each product absorbs properly.
Knowing about product categories helps you create an effective routine:
- Humectants draw water into your skin from the environment and deeper skin layers
- Emollients soften and smooth the skin surface by filling gaps between cells
- Occlusives create a protective seal that prevents water loss throughout the day
Using a humidifier in dry climates helps maintain moisture. Avoid excessive air conditioning or heating that depletes humidity.
Beneficial Components for Barrier Recovery
Certain ingredients target skin barrier repair. Ceramides are key in rebuilding the lipid matrix that holds skin cells together.
Fatty acids like linoleic and oleic acid provide structural support. They work with cholesterol to create a protective layer. Together, they help your skin function properly.
Niacinamide stimulates your skin’s natural ceramide production. It encourages your skin to make its own protective components. Studies show it improves barrier function over time.
Hydration-focused ingredients complement lipid restoration:
- Hyaluronic acid holds up to 1,000 times its weight in water, providing intense hydration
- Glycerin attracts moisture from the environment and deeper skin layers
- Peptides support the structural proteins that maintain skin integrity
When introducing new ingredients, start with one at a time. Wait at least two weeks before adding another. This approach prevents overwhelming your skin and helps you find what works best.
Consistency is more important than quantity. Using a few well-chosen products regularly is better than rotating through many. Your skin barrier repair depends on sustained support.
Substances That Compromise Healing
Knowing what to avoid is key. Harsh sulfates in cleansers strip away natural oils. Use soap-free cleansers for sensitive skin instead.
Fragrance and essential oils can irritate compromised barriers. While they create pleasant scents, they often contain chemicals that stressed skin can’t tolerate. Opt for fragrance-free products.
Denatured alcohol in high concentrations quickly evaporates, removing moisture from your skin. Be cautious of products with alcohol listed among the first five ingredients.
Physical exfoliants can cause micro-tears in compromised skin. Chemical exfoliants with mild alpha hydroxy acids provide gentler alternatives that remove dead skin without mechanical abrasion. Exfoliate no more than once or twice weekly during barrier repair.
Cleansing technique is important. Massage cleanser onto your face briefly and rinse without prolonged rubbing. Over-cleansing removes protective oils, even with gentle products. Limit face washing to twice daily at most.
pH balance is critical. Healthy skin has a slightly acidic pH around 5.5. Alkaline cleansers can disrupt this balance and compromise barrier function. Choose pH-balanced products when possible, during recovery periods.
Context determines whether an ingredient is harmful. Some actives that benefit healthy skin may irritate compromised barriers. Concentration levels matter—a small amount might help while higher concentrations cause problems.
Be patient with barrier restoration. Most people see noticeable improvement within three to four months of consistent care. This timeline reflects how long your skin needs to regenerate its protective lipid layers. Patience and persistent attention to supportive practices yield the best long-term results.
The Importance of a Customized Skincare Routine
Creating a skincare routine that works for you means understanding your skin better than any generic advice. What helps your sister’s dry patches might cause breakouts on your skin. The expensive serum your coworker loves might sting your sensitive skin.
Effective skin barrier repair doesn’t fit everyone. Your skin reacts differently to things than others do. Learning to understand these reactions helps you build a routine that supports your skin, not hinders it.
The journey to healthier skin starts with paying attention to your skin’s signals. Notice how your skin feels throughout the day and after using different products. This awareness is key to making choices that meet your specific needs.
Understanding Your Individual Skin Characteristics
Your natural skin type—whether oily, dry, combination, or sensitive—is the starting point for choosing products. These qualities affect how your skin handles oils, moisture, and ingredients. But, barrier damage can change these traits in unexpected ways.
Oily skin with barrier damage often feels dry, not just oily. The surface may feel slick, but deeper layers lack moisture. Dry skin with a damaged barrier may feel extremely tight and flaky, even with regular moisturizers.
These changes require adjusting your routine, even if it seems counterintuitive. An oily-skinned person might need richer hydration during barrier recovery. Someone with naturally dry skin might benefit from lighter layers that don’t overwhelm sensitized tissue.
Your skin type changes over time. Hormonal shifts, climate changes, and aging all affect how your skin behaves. Products that worked five years ago may not be right now. Regularly checking your routine helps you stay in tune with your skin’s current needs.
Building Sustainable Daily Practices
Consistency is key to supporting barrier health. Your skin prefers steady, appropriate care over sporadic use of high-end products. Think of skincare like nutrition—regular, balanced care produces better results than occasional elaborate treatments.
Start with basic essentials that you can maintain long-term. A gentle cleanser, appropriate moisturizer, and sun protection are the core of effective barrier support. Add complexity only when you can sustain it and when your skin genuinely needs it.
The best products are those you’ll actually use every day. Affordability, accessibility, texture preference, and personal tolerance all influence consistency. A drugstore moisturizer applied faithfully twice daily outperforms a luxury cream used sporadically because it feels too precious to use regularly.
Skin barrier repair takes months, not weeks. Visible improvement requires patience and persistence, even when you don’t see immediate changes. The protective lipid layers rebuild gradually through consistent support, not dramatic interventions.
Common obstacles like travel, schedule changes, or product confusion can disrupt routines. Plan for these challenges by keeping travel-sized essentials packed, choosing products with multi-use purpose, and simplifying your routine to its most critical steps during busy periods.
Adapting to Changing Conditions
Your skin’s needs change with circumstances, requiring routine flexibility. Seasonal changes are the most predictable adjustments. Winter often demands richer moisturizers and more frequent application. Summer humidity might allow lighter formulations that won’t feel heavy in the heat.
Life stage transitions also influence barrier requirements. Hormonal shifts during puberty, pregnancy, or menopause change how skin produces oil and retains moisture. These periods may reveal signs of skin barrier breakdown that weren’t present before, requiring modified support strategies.
Environmental transitions matter too. Moving from a humid coastal climate to a dry inland region changes your skin’s moisture loss rate. Your previous routine might suddenly feel insufficient in the new environment.
Health-related factors require consideration as well. Certain medications affect skin hydration and sensitivity. Stress periods can temporarily increase reactivity. These situations call for gentler products and extra barrier support until conditions normalize.
Evaluate your routine regularly by observing your skin’s responses. Notice what’s working well and what seems less effective. Make one change at a time so you can assess its impact accurately. Give each adjustment several weeks before adding more changes.
- Monitor how your skin feels in the morning and evening
- Track which products consistently improve comfort and appearance
- Note any reactions or increased sensitivity to specific ingredients
- Adjust product weight (richer or lighter) based on seasonal changes
- Revisit your routine every few months to ensure it matches your needs
Flexibility within consistency represents the ideal balance. Maintain your core beneficial practices—gentle cleansing, adequate moisturization, sun protection—while adjusting specific products or application frequency as conditions warrant. This approach provides stability without rigidity.
Learning your skin’s language takes time and attention. You become the expert on your own skin through careful observation and thoughtful adjustments. This knowledge serves you better than following universal prescriptions that ignore individual variation.
The most effective skincare routine is the one tailored to your specific skin, affordable enough to maintain, and simple enough to follow consistently. Focus on these practical realities, not trends or expensive recommendations that don’t align with your actual needs and circumstances.
When to Consult a Dermatologist
Sometimes, skin problems need a doctor’s check-up. For mild issues, home care works well. But, if symptoms don’t go away or get worse, see a dermatologist. They are experts in treating complex skin issues.
Signs that Require Professional Attention
If symptoms last over a month, even with good care, see a doctor. Sudden dryness or redness needs a check-up. Signs of infection or painful cracks are urgent.
Itching that keeps you awake also means you need help. Skin problems can get worse without the right treatment.
What to Expect During a Consultation
Your dermatologist will look at your health history and skincare routine. They’ll check your skin and might do tests. Patch tests and biopsies are sometimes needed.
Bring your skincare products and photos of your skin. This helps your doctor understand your situation better.
Follow-up Care and Treatment Options
Doctors often prescribe stronger products for your skin. They might give you creams to reduce inflammation. They’ll also suggest treatments for underlying issues.
Follow-up visits are important to see how you’re doing. It may take months to see improvements. Working with your doctor and taking care of your skin at home is key.
Always see a board-certified dermatologist or a qualified healthcare professional for the right diagnosis and treatment. This content is for informational and educational purposes only and does not constitute medical advice.


