In the United States, up to 33% of people with darker skin tones see patches of facial skin discoloration. This is similar to melasma, as reported by the American Academy of Dermatology. Many look for a guide to spot melasma early and avoid mistakes.
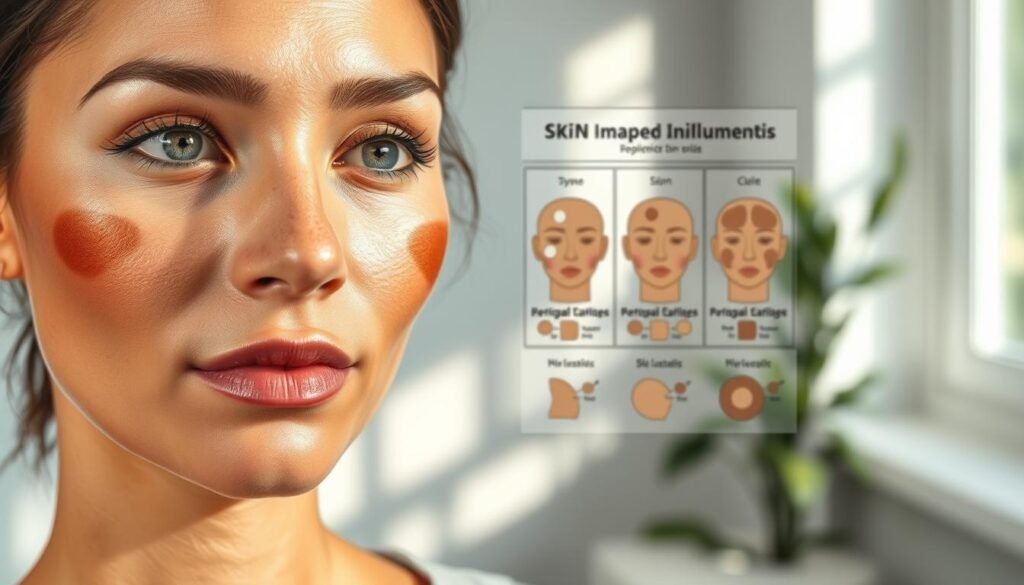
This guide starts with the basics. You’ll learn the first signs of Melasma and Hormonal Pigmentation. You’ll also know where it usually shows up and how daily habits can make it more noticeable. Look for brown or grayish patches on the cheeks, forehead, upper lip, chin, and nose.
Melasma is linked to hormones and UV light. It can be triggered by sun exposure, blue light from screens, and hormonal changes. Experts in United States skincare often recommend sunscreen, shade, and gentle routines while you seek a diagnosis.
While melasma can last and change with the seasons, this guide makes it simple. You’ll learn what patterns to watch, how to track changes, and when to see a dermatologist. This guide helps you understand melasma without confusion. The information here is not meant to diagnose, treat, cure, or prevent any disease. Always get professional medical advice before changing your skincare or health routine.
Key Takeaways
- Melasma often shows as brown or grayish patches in a symmetrical pattern on the face.
- Common triggers include sunlight, blue light, and hormonal shifts like pregnancy or birth control.
- Melasma and Hormonal Pigmentation are related, but melasma is a hormone- and UV-influenced subtype of hyperpigmentation.
- Track when patches darken during seasons, travel, or daily habits to spot patterns.
- Use sun protection and gentle care while you arrange a dermatologist visit for confirmation.
- This informational how-to guide focuses on practical steps for United States skincare needs.
What is Melasma?
Melasma is a common skin issue that causes brown or gray patches on the face. These patches often appear on the cheeks, forehead, and nose. They can also show up on the neck or forearms. Sun exposure and hormonal changes are common causes.
Anyone can get melasma, but it’s more common in women and those with darker skin. It’s not harmful but can affect how you feel about your skin. It might change your daily routines and choices.
Definition and Characteristics
Melasma is a condition where the skin produces too much melanin. This leads to skin discoloration that can change with heat, light, or stress. When you’re exposed to less of these, the patches can lighten.
The patches are often symmetrical and can range from tan to slate in color. They can become more visible with more sun exposure.
Types of Melasma
There are two main types of melasma. Patchy melasma has larger, irregular patches. Spotted melasma, or hormonal melasma, has many small spots.
Some people have a mix of both. The appearance can change based on sun exposure, skincare, and hormonal shifts.
Common Symptoms
Common signs include brown or gray patches that look the same on both sides of the face. Patchy melasma has blurry edges, while spotted melasma has distinct dots. The skin looks even but mottled.
Hormonal changes can happen with melasma. This includes changes in menstrual cycles, sleep, fatigue, acne, or appetite. Everyday light, heat, and pollution can make the patches more noticeable.
| Feature | Patchy Pattern | Spotted Pattern | Shared Traits |
|---|---|---|---|
| Appearance | Large, irregular areas | Multiple small spots | Tan to slate tone |
| Distribution | Cheeks, forehead, upper lip | Cheeks, temples, jawline | Often symmetrical facial patches |
| Borders | Soft, blurred edges | More defined speckles | Blend with surrounding skin |
| Triggers Noted in Practice | Sun and heat exposure | Hormonal shifts and light | Melasma causes include UV, hormones, and irritation |
| Sensory Changes | Typically none | Typically none | Cosmetic concern without pain or itch |
Understanding Hormonal Pigmentation
Hormonal pigmentation happens when hormones change how skin makes melanin. It shows up as brown patches that get darker with sun exposure. To tackle this, it’s key to watch for life changes and sun habits.
Dermatology guidance often notes that estrogen and progesterone can affect melanin. When these hormones change, skin reacts more to light. This makes it harder to remove pigmentation without proper care.
What Causes Hormonal Pigmentation?
Estrogen usually keeps melanin in check. But when estrogen levels drop or change, melanin increases. This can happen during pregnancy, after having a baby, or during menopause.
Hormonal birth control can also cause color changes. This includes pills, IUDs, and implants. Hormone therapy and irregular cycles can also play a role. UV and visible blue light can make it worse, even through windows.
- Life stages: pregnancy “mask,” postpartum shifts, midlife transitions
- Medications: combined pills, progestin-only methods, or hormone therapy
- External drivers: high sun, visible light, and heat exposure
- System stressors: prolonged stress that disrupts endocrine rhythm
Many seek remedies for hormonal pigmentation. They focus on sun protection and consistent routines. These steps help manage the condition without aggressive treatments.
Symptoms to Watch For
Look for symmetrical patches on the cheeks, temples, or forehead. The edges may be soft and spread slowly. The color can range from light tan to deep brown and darken after sunny days.
Also, watch for signs of hormonal imbalance: irregular periods, poor sleep, fatigue, appetite swings, or breakouts. Changes like starting birth control, seasons changing, or rising stress can make pigmentation more noticeable.
| Symptom Pattern | Typical Locations | Common Triggers | Helpful First Steps |
|---|---|---|---|
| Symmetrical brown patches | Both cheeks, temples, forehead | UV/visible light, heat | Daily SPF 30+, wide-brim hat |
| Gradual darkening after routine changes | Cheekbones, upper lip | New contraceptive, hormone therapy | Discuss timing with a clinician |
| Seasonal flare-ups | Forehead, nose bridge | Summer sun, outdoor sports | Reapply sunscreen every 2 hours |
| Linked systemic signs | Face with occasional jawline acne | Stress, irregular cycles, poor sleep | Stress management, sleep hygiene |
| Persistent patches despite care | Cheeks with expanding edges | Ongoing light exposure | Seek hormonal pigmentation remedies with professional guidance |
The Link Between Melasma and Hormones
Changes in our body’s chemistry can affect our skin. Many cases of melasma are linked to hormonal shifts. These changes, combined with sunlight, can darken skin on the cheeks, forehead, and upper lip.
Hormonal Triggers
Pregnancy, the postpartum period, perimenopause, and menopause can trigger melasma. Birth control pills and hormone therapy can also increase sensitivity to hormones. Stress adds to the mix, causing cortisol levels to fluctuate.
Two people on the same birth control can react differently. Some see faint patches that fade, while others develop thick, dark spots. The severity depends on season, location, and sun exposure.
How Hormones Affect Skin Pigmentation
Estrogen helps control melanocyte signals. When estrogen levels drop or change, melanocytes can produce more melanin. This makes normal sunlight a trigger for melasma, affecting exposed skin.
Progesterone changes can also affect how skin responds. This is why hormonal imbalances often worsen during certain life stages. Treatment plans need to consider these hormonal shifts.
| Life Stage or Factor | Hormonal Shift | Impact on Pigment | Real-World Example |
|---|---|---|---|
| Pregnancy | Rising estrogen and progesterone | Higher melanocyte activity on sun-exposed areas | “Mask of pregnancy” darkens after brief morning walks |
| Postpartum | Rapid hormone decline | Rebound in signaling pathways tied to melasma causes | Patches persist as sleep loss and stress extend recovery |
| Perimenopause/Menopause | Fluctuating then reduced estrogen | Inconsistent pigment response with UV synergy | Uneven spots appear despite cloudy-day commutes |
| Hormonal Birth Control | Exogenous estrogen/progestin | Estrogen progesterone sensitivity may increase | New patches form after starting a combined pill |
| Hormone Therapy | Adjusted sex hormone levels | Variable melanocyte stimulation | Tone shifts with dose changes under medical care |
| Chronic Stress | Cortisol fluctuations | Amplifies a hormonal imbalance skin issue | Work strain coincides with stubborn darkening |
Risk Factors for Developing Melasma
Several factors contribute to melasma. Genetics, light, heat, and hormonal changes all play a role. In the United States, sun exposure varies by region and season, making sun-induced hyperpigmentation worse. Daily habits, products, and environmental factors also impact outcomes.
Genetics
Family history is a strong indicator. People with olive to darker skin, like those from Latin American, African, Middle Eastern, or Asian backgrounds, are more likely to get it. Women often see more flare-ups, and their genes can make them more sensitive to light and heat.
These risk factors can lead to melasma early in adulthood. If your relatives have persistent patches, watch for changes during seasonal shifts and life events.
Sun Exposure
UV rays and visible blue light activate melanocytes, making patches darker. In the United States, sun exposure peaks in spring and summer. Outdoor jobs and travel to high-UV areas can also speed up hyperpigmentation.
Smog and smoke can make existing discoloration worse. Using strong peels or acids too much can thin the skin, increase photosensitivity, and make patches more noticeable.
Hormonal Changes
Pregnancy, the postpartum period, perimenopause, and menopause can change hormone levels and affect melanin production. Starting or changing hormonal contraceptives, like those with more progestin, can also make pigment more intense.
Irregular cycles and stress can lead to more color in the skin. Heat, indoor lighting, and other environmental factors can darken patches throughout the day.
| Trigger | How It Raises Risk | Typical Situations in the U.S. | What to Watch |
|---|---|---|---|
| Genetic Predisposition | Inherited traits increase melanocyte reactivity | Family clusters among women with medium to dark tones | Early patches after minor sun or heat |
| United States Sun Exposure | UV and blue light trigger melanin production | Summer peaks, Southern and high-altitude regions, beach travel | Seasonal darkening and larger patch edges |
| Hormonal Shifts | Estrogen and progesterone influence melanogenesis | Pregnancy, postpartum, contraceptive changes, perimenopause | New patches across cheeks, forehead, or upper lip |
| Environmental Factors | Pollution and heat amplify visible discoloration | Urban smog, hot kitchens, gyms, and steam rooms | Deeper tone after heat or high-traffic commutes |
| Barrier Disruption | Harsh acids heighten photosensitivity | Frequent high-strength peels and exfoliants | Patch darkening despite routine sunscreen |
How to Identify Melasma
Start by looking closely in bright, indirect light. Pay attention to sun-exposed areas. Look for consistent skin discoloration patterns that resemble melasma and hormonal pigmentation.
Visual Inspection Techniques
Check the cheeks, forehead, upper lip, and chin for brown or grayish-brown patches. Melasma often shows up symmetrically on both sides of the face. Also, check temples and sometimes the neck or forearms.
Notice the border style and size. Patchy areas have soft, blurred edges. Spotted patterns have uneven dark dots. Compare these to clear skin to see color depth and edge clarity.
Examine in daylight near a window or with a bright, diffused lamp. Turn your face side to side to see how the tone changes. This helps map skin discoloration patterns linked to melasma and hormonal pigmentation.
Self-Examination Tips
Keep track of when patches darken. Note changes after sun exposure, during pregnancy, or after starting birth control. Also, log seasonal shifts, outdoor time, and sunscreen habits from brands like CeraVe, La Roche-Posay, or Neutrogena.
Avoid over-exfoliation, harsh scrubs, or frequent strong peels. These can make melasma look worse. Distinguish from post-inflammatory marks, which are often scattered, asymmetrical, and follow acne or minor injuries.
If coverage seems to spread or deepen even with steady SPF use and shade practices, document changes with clear photos in the same light. This record clarifies skin discoloration patterns and supports an informed talk about melasma and hormonal pigmentation with a licensed dermatologist.
Diagnosing Hormonal Pigmentation
Getting a clear diagnosis is key. It helps tell melasma apart from hyperpigmentation and finds out what causes them. In the United States, doctors look at color, symmetry, and where the spots are before they start treatment.

Consultation with a Dermatologist
A board-certified doctor will look at your medical history. They check for things like pregnancy, birth control, hormone therapy, and stress. They also look at how the spots compare to others on your body.
They pay special attention to if the spots are on both sides of your face. This helps them figure out if it’s melasma or something else. It also makes sure they follow the right standards in the United States.
Recommended Tests
Doctors often use tests to get a better look. A Wood’s lamp shows how deep the spots are. Dermoscopy helps see the details of the spots. This helps the doctor plan the best treatment.
If hormones might be the cause, the doctor might work with other doctors. This team approach is common in the United States. It makes sure the treatment is right for the problem.
Treatment Options for Melasma
Melasma needs a careful, layered approach. A good plan might include a doctor’s advice, daily habits, and occasional in-office treatments. Hormones often play a big role, so results may take time.
Topical Treatments
Home care often starts with a strong pigmentation cream. Ingredients like hydroquinone, tretinoin, and mild corticosteroids are common. Vitamin C or azelaic acid may also be added for extra protection.
Results can vary. Melasma can be hard to treat, so consistent use and sun protection are key. Always use a daily SPF 30 or higher and gentle cleansers to keep your skin healthy.
Professional Procedures
Clinics might use lasers or light devices to target pigment. The timing and settings are very important. A dermatologist will consider your skin type, season, and sun exposure.
Strong peels or too many sessions can make your skin more sensitive to the sun. Experts often use different treatments together. This helps remove pigment slowly and avoids darkening.
Lifestyle Changes
Protecting your skin from the sun is essential. Use sunscreen, stay in the shade, and wear hats during peak sun hours. These habits help any treatment work better and prevent flare-ups.
Choose gentle products and avoid harsh scrubs. Managing stress, getting enough sleep, and talking to your doctor about hormones are also important. Good nutrition and ongoing care can help keep your skin looking better.
| Approach | Primary Goal | Best For | Key Actives/Methods | Pros | Considerations |
|---|---|---|---|---|---|
| Topicals at Home | Lighten and stabilize | Mild to moderate patches | Hydroquinone, tretinoin, vitamin C, azelaic acid | Accessible, adjustable, supports long-term care | Needs consistency; irritation risk if overused |
| In-Office Devices | Target excess pigment | Stubborn or recurrent cases | Low-energy lasers, gentle light-based therapy | Faster visible change in select patients | Must be customized; sun timing matters |
| Conservative Peels | Improve tone and texture | Carefully selected candidates | Superficial acids in cautious protocols | Can boost topical results | Strong peels can worsen melasma |
| Lifestyle Measures | Prevent triggers and relapse | All skin types | Broad-spectrum SPF, shade, hats, gentle skincare | Essential foundation for every plan | Requires daily discipline |
| Medical Guidance | Personalized oversight | Complex or hormonal cases | Dermatologist recommended treatment plans | Tailored and monitored | Regular follow-up needed |
Managing Hormonal Pigmentation
When hormonal imbalances cause melasma, careful habits and smart choices help. Daily protection and the right treatments, with medical advice, create effective solutions for hormonal pigmentation. These solutions fit into our everyday lives.
Consistency matters. Keeping a steady skin care routine for melasma prevents flare-ups. It keeps results stable all year round.
Hormone Therapy Considerations
Talk to your doctor if melasma patches appear or darken after starting birth control or hormone therapy. Changes in estrogen and progestin can affect pigment. Some cases start two to three months after starting progestin-containing contraceptives.
During perimenopause and menopause, you might need special adjustments. Don’t change your medication without your doctor’s okay. Discuss options, timing, and dosage to match your health goals.
Supportive steps help too. Reducing stress, getting enough sleep, and exercising regularly can help steady hormone signals. This complements melasma management under your doctor’s care.
Skin Care Regimens
Wearing daily broad-spectrum sunscreen is essential. Reapply when outdoors and use hats and UPF clothing. Visible light is important; consider mineral formulas with iron oxides for your skin care routine.
Choose a gentle cleanser and a moisturizer with ceramides or squalane. Add brighteners like azelaic acid, niacinamide, kojic acid, or Vitamin C serum. Avoid over-exfoliating and strong peels that can make hormonal imbalances worse.
Expect ongoing care. Melasma management often requires long-term, consistent effort. Make seasonal adjustments—stronger protection in spring and summer, and antioxidants all year—to keep results steady.
| Focus | Action | Why It Helps | Practical Picks |
|---|---|---|---|
| Sun Defense | Apply SPF 50+, reapply every 2 hours outdoors | Blocks UV and visible light that trigger pigment | Mineral SPF with zinc oxide and iron oxides |
| Barrier Care | Use gentle cleansers and rich moisturizers | Reduces irritation that can darken spots | Ceramides, glycerin, squalane |
| Brightening | Layer proven agents in low, steady doses | Targets excess melanin without harsh peeling | Azelaic acid, niacinamide, kojic acid, Vitamin C |
| Hormonal Review | Consult on contraception or hormone therapy timing | Aligns care with a hormonal imbalance skin issue | Physician-guided adjustments, stress management |
| Lifestyle | Plan seasonal shifts and protective clothing | Limits flare-ups and supports melasma management | UPF hats, sunglasses, midday shade |
| Consistency | Maintain a daily skin care routine for melasma | Turns short-term gains into lasting control | AM: sunscreen + antioxidants; PM: gentle brighteners |
Prevention Strategies for Melasma
Daily habits shape outcomes. Focus on sun protection for melasma and consistent care for hyperpigmentation prevention. Small, steady steps help prevent skin discoloration all year round.

Sun Protection Tips
Apply a broad-spectrum SPF 30 or higher every morning, even on cloudy days. Reapply every two hours outdoors and after swimming or sweating. Stay in the shade from 10 a.m. to 4 p.m. and avoid tanning beds to prevent skin discoloration.
- Wear a wide-brim hat, UV-blocking sunglasses, and UPF clothing for extra sun protection for melasma.
- Be careful during high-altitude trips and beach days, where UV and visible light are stronger.
- Layer antioxidants under sunscreen to help with hyperpigmentation prevention when pollution and heat rise.
Plan your day around sun exposure—commutes, school runs, or outdoor sports. When darkening starts, act early with shade, reapplication, and coverage. For more guidance, see this practical overview on how to reduce dark spots and.
Importance of Skincare Routine
The importance of skincare routine lies in consistency. Cleanse gently, repair the barrier with ceramides, and apply vitamin C or niacinamide in the morning. At night, use dermatologist-approved lightening agents as directed to prevent hyperpigmentation.
- Avoid harsh scrubs and aggressive peels that can trigger irritation and increase photosensitivity.
- Track triggers like heat, sweat, and blue light from devices; adjust sunscreen and coverage as needed.
- Consult a board-certified dermatologist to tailor sun protection for melasma and guide prevention of skin discoloration.
Keep products simple and stable, and patch test new formulas before full use. A calm, protected skin barrier improves outcomes and supports the importance of skincare routine over time.
When to Seek Professional Help
Not sure when to see a dermatologist for dark patches on your face? Watch for changes over time. If spots spread or deepen in color, despite using SPF 30+ and wearing hats, it’s time to visit a dermatologist. Also, if new pigmentation appears during pregnancy or after starting birth control, seek help.
Redness, burning, or peeling from harsh routines may indicate treatment-resistant pigmentation. This condition needs safer care.
Signs Melasma Needs Treatment
Seek care if over-the-counter serums don’t work after two to three months. If patches look uneven, sharply edged, or asymmetrical, it’s a sign. Also, rapid change, irritation after peels, or color that doesn’t fade with sun protection are red flags.
These signs tell you it’s time to see a dermatologist before the condition worsens.
Importance of Expert Diagnosis
An expert diagnosis can rule out other conditions like post-inflammatory marks or drug-induced pigmentation. A dermatologist will recommend a treatment plan. This may include hydroquinone, azelaic acid, retinoids, and short courses of steroids.
They will also suggest gentle cleansers, moisturizers, and daily zinc oxide sunscreen. In some cases, low-fluence lasers or carefully selected peels are recommended. These treatments aim to protect the skin barrier and prevent rebound.
Because hormones and UV both fuel relapse, a long-term strategy is key. Your dermatologist can tailor a maintenance plan. They will also coordinate with your OB-GYN or primary care on contraceptive options. This guidance helps avoid setbacks, supports safer choices, and improves outcomes over time.