Did you know that over 60% of people experience signs of compromised skin health at some point in their lives? Your outer layer works tirelessly to protect you every single day. When it becomes weakened, you might notice changes that affect how your face and body look and feel.
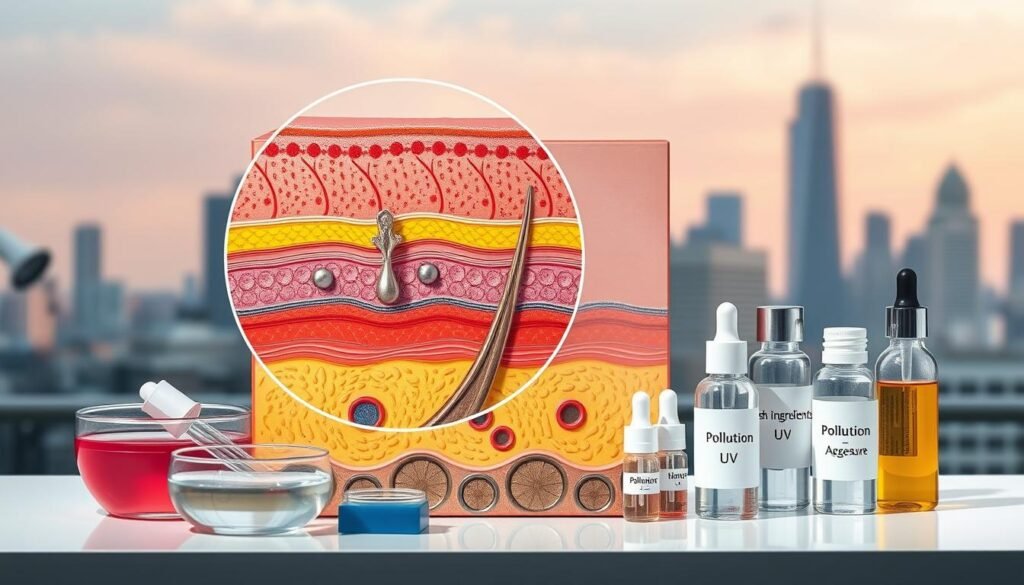
Your protective layer is made up of the stratum corneum. This outermost section includes corneocytes arranged like bricks in a wall. Between these cells sit lipids such as ceramides, cholesterol, and fatty acids that act as mortar.
This structure keeps water inside while blocking harmful chemicals and bacteria from entering. When this defense system becomes compromised, you may experience discomfort and visible changes.
Important note: This article provides educational information only. It cannot diagnose conditions or replace professional medical advice. Everyone’s body responds differently to environmental factors, lifestyle choices, and aging. If you have concerns about persistent symptoms, consult a dermatologist for personalized evaluation.
Throughout this guide, you’ll learn to identify common signs, understand contributing factors, and gain knowledge about what healthy protection looks like.
Key Takeaways
- Your outer protective layer consists of cells and lipids working together like bricks and mortar to shield your body from external threats.
- Over 60% of people experience some form of compromised skin health during their lifetime due to various factors.
- Common signs include dryness, redness, itching, flaking, and increased sensitivity to products or environmental conditions.
- Multiple factors contribute to weakness, including weather changes, harsh products, over-cleansing, and natural aging processes.
- This article serves educational purposes and cannot replace professional dermatological evaluation or diagnosis.
- Individual experiences vary significantly, and persistent symptoms may indicate underlying conditions requiring medical attention.
- Learning to recognize early warning signs helps you take proactive steps toward maintaining healthier, more resilient protection.
Understanding the Skin Barrier
Your skin works hard every day to keep you safe and hydrated. It protects your body from harm while keeping moisture in. Knowing how it works helps you spot problems early.
The skin barrier is your body’s first defense against the outside world. Learning about its structure and function helps you act fast when your skin health is at risk.
The Protective Outer Layer
Your skin barrier has the stratum corneum, the outer layer of your skin. It’s made of dead cells that protect the living skin underneath.
This layer is like a brick wall with dead cells as bricks. Lipids like ceramides and cholesterol act as mortar, keeping the barrier strong. This keeps harmful stuff out of your skin.
The lipids in the barrier work together to keep it tight. When it’s intact, your skin stays hydrated and protected.
| Component | Function | Impact on Barrier Health |
|---|---|---|
| Corneocytes | Structural cells forming protective barrier | Provide physical defense and structural integrity |
| Ceramides | Lipids binding cells together | Maintain moisture retention and barrier cohesion |
| Cholesterol | Lipid supporting membrane fluidity | Ensures flexibility and repair capacity |
| Fatty Acids | Natural oils sealing gaps | Prevent transepidermal water loss |
Why Barrier Health Matters
A healthy moisture barrier does two important things. It keeps water in and keeps bad stuff out. This keeps your skin hydrated and safe.
Your barrier controls how much water your skin loses. When it works right, your skin stays moist and healthy. It also keeps your skin’s pH balanced, making it hard for bad bacteria to grow.
The skin barrier helps your immune system by keeping out allergens and germs. It filters out pollutants and bacteria every day. When it’s strong, your skin looks and feels great.
But if your barrier is weak, you can get dry, irritated skin. It can’t keep moisture in, and bad stuff can get in. This leads to inflammation and discomfort.
Knowing how your skin barrier works helps you catch problems early. Understanding normal function is key to spotting when something’s wrong. This knowledge is vital for catching damage before it gets worse.
Common Signs of a Damaged Skin Barrier
When the skin’s protective shield breaks down, you’ll notice visible and tactile symptoms. These signs can affect how your skin looks and feels. Knowing these warning signs helps you take action early to prevent problems from getting worse.
Common signs include discomfort, texture changes, and sensitivity to products. These symptoms often appear together. Recognizing these signs helps you care for your skin properly.
Redness and Inflammation
A damaged barrier can cause your skin to become red and inflamed. Without protective lipids, your skin can’t defend against irritants. This leads to red patches and facial flushing.
Redness from cold weather or exercise is different from chronic inflammation. Chronic redness means your barrier is not working right. It may be a sign of deeper issues that need a doctor’s attention.
Dryness and Flakiness
Damage to the barrier can cause your skin to lose moisture. This makes your skin feel tight and dry, even after moisturizing. Your skin’s inability to hold moisture is a sign of barrier damage.
Visible flaking and scaling are signs of severe dehydration. These symptoms show that your barrier is not doing its job. You need to take action to restore moisture.
- Persistent tightness that worsens throughout the day
- Rough patches that feel like sandpaper to the touch
- Visible flaking despite consistent moisturizer use
- Skin that absorbs products immediately without lasting hydration
Increased Sensitivity
An intact barrier protects nerve endings from external stimuli. Damage makes these receptors more sensitive. Even gentle products can cause stinging or burning.
Many people feel discomfort when using products on damaged skin. This discomfort can range from mild to severe. It’s a sign that your barrier is not doing its job.
Other signs of barrier damage include itchiness, tenderness, and breakouts. You may also notice small bumps or texture changes. If these symptoms last or get worse, it’s time to see a dermatologist.
Visual Indicators of Skin Barrier Damage
Changes in your skin’s texture and look show barrier damage. When ceramides, fatty acids, and cholesterol are lost, your skin’s outer layers change. Spotting these signs early helps fix barrier dysfunction before it gets worse.
A damaged barrier lets moisture escape and lets in harmful stuff. This causes dehydration and visible signs. It also lets bacteria and pollution in, leading to inflammation and breakouts.
Appearance of Fine Lines
Dehydration makes fine lines more noticeable. When your barrier can’t hold moisture, your skin loses its plumpness. This leads to shadows and creases.
Dehydration lines are different from true aging wrinkles. They look like fine lines when your skin is dry. They show up more around your eyes, forehead, and mouth.
Dehydration lines can improve with epidermal recovery. Fixing your barrier and keeping moisture in can make them less visible. But, true wrinkles from aging or sun damage don’t change with just hydration.
If your skin looks more lined than before, it might be barrier damage. This sudden change means your skin needs barrier support and hydration right away.
Texture Changes and Bumps
Barrier damage shows in skin texture changes. Your skin might feel rough and have uneven surfaces. This is because damaged barriers mess up cell turnover.
When barriers are damaged, dead skin cells don’t shed right. This leads to buildup and rough patches. Your skin looks bumpy and different from usual.
Small bumps can look like acne but are actually from barrier damage. They come from:
- Cell buildup from bad desquamation
- Bacteria getting in and causing inflammation
- Clogged pores from debris and oil flow issues
- Sensitivity to products that used to be okay
These bumps often show up in dry or stressed areas. They’re common on cheeks, jawline, and nose.
Spotting these signs early helps fix your skin faster. The sooner you act, the better. This stops mild issues from turning into big problems.
Factors Contributing to Skin Barrier Damage
Barrier damage often comes from many sources. Your skin faces challenges from the environment, products, and daily choices. Knowing these factors helps you protect your skin better.
There are three main causes of skin barrier damage. Each plays a unique role in weakening your skin. Understanding these helps you make better choices for your skin.
External Threats to Barrier Integrity
Environmental factors stress your skin, weakening it over time. UV radiation is a big threat. It breaks down the lipids and proteins in your skin, creating gaps in your defense.
Pollution and airborne particles cause inflammation. These invaders damage your skin’s barrier. People in cities often face more damage due to pollution.
Extreme temperatures make your skin work harder. Cold weather reduces blood flow to skin cells. Heat causes water loss, drying out your skin.
Low humidity environments are a big problem in winter. Indoor heating takes moisture from the air, drying your skin. Wind also removes protective oils from your skin.
These environmental attacks add up over time. Daily exposure weakens your skin’s repair ability. Protecting your skin consistently is key to maintaining health.
How You Care for Your Skin Matters
Skincare habits are a big problem for barrier damage. Over-cleansing removes natural oils that protect your skin. Washing your face too much removes these oils faster than your body can replace them.
Harsh surfactants and alkaline soaps disrupt your skin’s pH balance. Your skin works best at a pH of 5.5. Products with pH above 7 harm the enzymes that make barrier lipids.
Excessive exfoliation also damages your skin. Scrubs and chemical exfoliants remove protective layers too quickly. Many think more exfoliation is better, but it’s not.
Here are some common practices that damage the barrier:
- Using hot water for cleansing, which dissolves barrier lipids
- Applying multiple active ingredients simultaneously without proper buffering
- Skipping moisturizer, which fails to supplement essential barrier components
- Layering incompatible products that increase irritation
- Not allowing sufficient time between introducing new products
Medical conditions can also weaken your barrier. Conditions like adult acne and atopic dermatitis require special care.
Daily Decisions That Affect Your Barrier
Lifestyle choices affect your skin’s repair. Inadequate sleep hampers repair during rest. Your skin repairs itself most between 10 PM and 2 AM.
Chronic stress triggers inflammation. Elevated cortisol levels harm barrier lipid production. This is why stress can lead to skin flare-ups.
Smoking and alcohol consumption harm your skin. Smoking reduces blood flow, depriving your skin of oxygen and nutrients. Alcohol dehydrates your skin by pulling water from cells.
Your diet impacts barrier repair. Lack of essential fatty acids, vitamins, and antioxidants limits repair. Processed foods with sugar can also trigger inflammation.
Identifying damage factors is the first step to prevention and repair. Most people find multiple factors weaken their barrier. Addressing these helps restore your skin’s natural protection.
The Role of Weather in Skin Health
Changing weather conditions challenge your skin barrier in unique ways. Different climates stress your skin barrier in different ways. Knowing these environmental factors helps you adjust your skincare routine all year.
Weather greatly affects your skin’s ability to protect itself. Seasonal changes cause predictable disruptions to your skin barrier. By recognizing these patterns, you can take steps to prevent damage.
Temperature and air moisture levels impact your skin’s hydration. The air around you constantly interacts with your skin barrier. This interaction affects whether your skin thrives or struggles.
Effects of Cold, Windy Climates
Winter weather is tough on your skin barrier. Cold air has less moisture, making environments dry. This dryness pulls water from your skin, speeding up moisture loss.
Harsh winds also strip away your skin’s natural oils. These oils protect your skin from water loss. Without them, your skin loses water quickly, becoming dry and depleted.
The switch between cold air and warm indoor spaces stresses your skin. This constant change weakens the proteins holding your skin cells together. Healing dry skin is harder in winter when these conditions are daily.
“Cold weather slows down the natural production of the lipids that form the skin barrier, making winter the most challenging season for maintaining healthy skin hydration.”
Exposed areas like your face and hands get very dry in cold, windy weather. They can become cracked and sensitive. It’s important to protect these areas to avoid long-term damage.
Impact of Humidity and Heat
Warm, humid weather affects your skin barrier differently than cold. While humidity helps keep moisture in, too much heat can cause problems. People often over-cleanse in warm weather, stripping their skin.
Air conditioning makes indoor spaces dry in summer. This dryness is similar to winter’s dryness. The contrast between humid outdoors and dry indoors stresses your skin barrier.
Sun exposure in warm weather damages your skin barrier. UV rays break down the lipids and proteins your skin needs. Protecting your skin from UV damage is key to keeping your barrier healthy and healing dry skin.
| Weather Condition | Primary Barrier Impact | Common Symptoms | Key Prevention Strategy |
|---|---|---|---|
| Cold, Windy Winter | Moisture depletion and lipid stripping | Severe dryness, cracking, flaking | Rich moisturizers with occlusive barriers |
| Hot, Humid Summer | Over-cleansing and UV degradation | Irritation, sensitivity, uneven texture | Gentle cleansing with broad-spectrum SPF |
| Indoor Climate Control | Low humidity causing dehydration | Tightness, dullness, fine lines | Humidifiers and hydrating serums |
Tropical or humid climates can hide barrier problems. Moisture can mask damage, allowing it to progress unnoticed. Problems become apparent when conditions change, revealing the true state of your skin barrier.
Adjusting your skincare routine to the seasons protects your skin barrier all year. Each climate has its own challenges that need specific solutions. Making proactive changes prevents damage that’s hard to fix later.
Lifestyle Factors Affecting Skin Barrier
Your lifestyle choices greatly affect your skin’s ability to repair and protect itself. Skin changes can happen for many reasons. Internal factors often play a bigger role than external treatments alone. Your daily habits are key to skin barrier repair from within.
Whole-body wellness and skin integrity are closely linked. What happens inside your body affects your skin’s outer layer. Understanding these internal influences helps you support barrier health better.
Nutritional Building Blocks
Your diet gives your skin the raw materials it needs to repair itself. Nutritional intake affects whether your body can produce the lipids and proteins for barrier function. Without enough nutrients, even the best skincare routine won’t work.
Essential fatty acids are vital for barrier health. Omega-3 and omega-6 fatty acids are key for sealing moisture and keeping irritants out. Your body can’t make these fats, so getting them from food is critical for skin barrier repair.
Antioxidants protect against oxidative stress that damages barrier components. Vitamins C and E neutralize free radicals. They also help produce collagen, keeping skin structure and resilience.
Vitamin A supports cell turnover. It helps your skin shed old cells and make new ones. This keeps your barrier fresh and functional, not thick and sluggish.
Hydration is also key for barrier maintenance. Drinking enough water keeps all skin layers moist. Even with good topical hydration, not enough water makes skin dry and vulnerable.
Inflammatory diets harm barrier health. Processed foods and high sugar intake trigger inflammation. This inflammation makes it hard for your skin to make ceramides and other protective components.
Eating anti-inflammatory foods helps your barrier from within. Diets rich in fruits, vegetables, and healthy fats reduce inflammation. This lets your body focus on maintaining and repairing skin structures.
The Sleep and Stress Connection
Stress and skin health have a bidirectional relationship many overlook. Chronic stress raises cortisol, which hurts barrier lipid production. It also increases inflammation in your body, including your skin.
Stress disrupts sleep, leading to barrier problems. Lack of sleep messes with the body’s repair processes. Your body regenerates barrier components and makes collagen at night.
Deep sleep stages are critical for skin barrier repair. Your body heals and regenerates during these phases. Transepidermal water loss increases during deep sleep as your skin focuses on repair.
Quality sleep is essential for barrier repair. Without enough rest, barrier components stay damaged and depleted. Poor sleep leads to increased sensitivity, dryness, and visible aging.
Managing stress helps sleep and barrier function. Lower stress means less cortisol, allowing normal lipid production. Better sleep lets your body make protective barrier elements.
Addressing lifestyle factors creates a better environment for barrier recovery. Topical treatments work better with proper nutrition, enough sleep, and managed stress. This whole-body approach gets results that surface treatments alone can’t.
The Influence of Aging on Skin
As we get older, our skin changes in ways that affect its health and function. These changes make it harder for our skin to protect itself, keep moisture, and heal from damage. Knowing how aging impacts our skin helps us adjust our skincare to meet our skin’s new needs.
The signs of aging show deeper changes in our skin’s structure. What worked well in our twenties may not be enough in our fifties and beyond.
Natural Aging Process
Our skin’s ability to protect itself naturally gets weaker with age. Ceramide synthesis decreases significantly as we age, affecting the lipid content that keeps skin cells together. This decline in lipid production is a key factor in barrier dysfunction.
Cell turnover slows down with age. In our twenties, our skin can quickly recover from daily washing. But by our fifties, sixties, or seventies, this process takes substantially longer.
Sebum production also decreases, which is more noticeable after menopause in women. This natural oil helps keep moisture in and adds protection.
The natural moisturizing factor components also decrease. These help the skin hold onto water. Changes in the dermis weaken the skin’s barrier, making it less resilient.
Changes in Skin Hydration
Keeping moisture in becomes harder as we age. Hyaluronic acid levels decrease, making it harder for the skin to hold water. This compound can hold up to 1,000 times its weight in water, making its decline significant.
Impaired barrier function means more water loss. Water evaporates more easily, leading to dehydration, even with enough water intake.
Mature skin has trouble keeping moisture in. Even with enough water, the visible signs of aging—like fine lines and loss of plumpness—get worse.
Your skincare routine needs to change with age. Focus more on hydration and moisturization to counteract these natural declines. Even rich products may become necessary as your skin’s repair abilities change.
| Skin Characteristic | Young Skin (20s-30s) | Mature Skin (50s-70s) | Impact on Barrier |
|---|---|---|---|
| Barrier Recovery Time | 6-7 hours after cleansing | 24+ hours after cleansing | Increased vulnerability to damage |
| Ceramide Production | High and consistent | Significantly reduced | Weakened lipid structure |
| Cell Turnover Rate | 28-35 days | 45-60 days | Slower barrier regeneration |
| Moisture Retention | Optimal hyaluronic acid levels | Depleted water-binding capacity | Chronic dehydration tendency |
Temporary versus Chronic Damage
Knowing if your skin damage is short-term or long-term is key to choosing the right treatment. Some skin problems fix quickly with the right care. But, others might show a deeper issue that needs a doctor’s help. Learning to tell the difference helps you take better care of your skin.
How you treat your skin changes based on whether the damage is temporary or chronic. Temporary issues might get better with good skincare. But, chronic problems often need special help.
Recognizing Temporary Issues
Temporary damage usually comes from a clear cause. Maybe you used a harsh product, stayed out too long in bad weather, or tried a cleanser that dried out your skin. These problems usually fix in days to weeks.
When the damage is temporary, your skin gets better with gentle care. You’ll see it improve as you use products that help your skin barrier. The symptoms will get better, not worse.
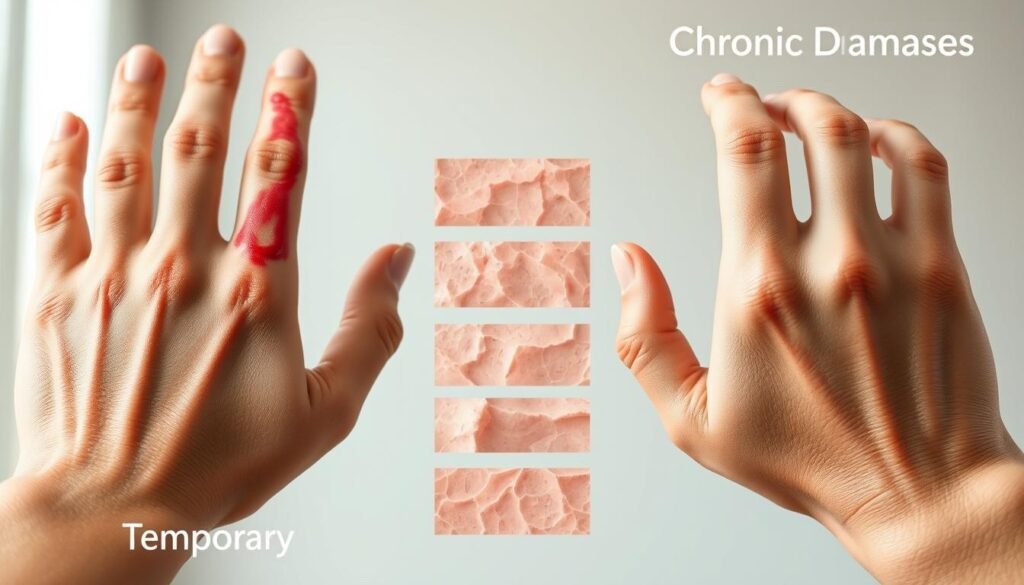
- Clear triggering event or product you can pinpoint
- Symptoms that improve within 1-2 weeks of supportive care
- Localized discomfort, not all over
- Healing happens slowly but steadily
- No history of similar problems coming back
Identifying Chronic Concerns
Chronic damage is different. It keeps coming back even with good care. It might mean you have a condition like atopic dermatitis, psoriasis, or rosacea. These need a doctor’s diagnosis and treatment.
Chronic damage doesn’t get better with just skincare. The symptoms might change but never really go away. You might keep getting flare-ups without a clear reason.
A damaged barrier can cause flaking and itching that won’t stop. This can lead to more problems like acne or eczema. These issues affect your daily life in big ways.
Signs of chronic damage include:
- Symptoms lasting more than 4-6 weeks, even with good care
- Same problems keep coming back
- Getting worse over time
- Problems happening all over your body
- Family history of skin problems like eczema
Determining When Professional Help Is Needed
Some dermatitis symptoms need a doctor right away, not just self-care. Knowing when to see a dermatologist is important. They can help prevent bigger problems and give the right treatment for your skin.
See a dermatologist if you have:
- Persistent symptoms that last more than 4-6 weeks, even with good skincare
- Severe symptoms like oozing, crusting, or skin that’s very hot
- Pain or signs of infection like pus or spreading redness
- Sudden changes in your skin without a clear reason
- Problems affecting your life like sleep, work, or daily activities
Also, see a doctor if you think you might have eczema, psoriasis, or rosacea. These need a proper diagnosis and treatment plan, not just general skincare.
This article is for education only and can’t diagnose medical conditions. Everyone’s skin reacts differently to treatments. A dermatologist can look at your symptoms, consider your health history, and suggest the best treatment for you.
Dermatologists have the tools and knowledge to help with complex skin problems. They can tell the difference between similar-looking issues and create a treatment plan just for you. Don’t hesitate to get expert advice if your skin problems keep coming back or getting worse, even with your best care.
Skincare Practices for Repairing the Barrier
Fixing your skin’s barrier needs gentle care and the right ingredients. When your barrier is damaged, every product and cleansing step is key. The key to fixing your skin barrier repair is to use practices that help, not harm your skin.
Your daily routine should aim to reduce irritation and boost hydration. This means changing habits that might harm your skin. Many people unknowingly damage their barriers by cleansing too much or using the wrong products.
Gentle Cleansing Methods
Cleansing is where most barrier damage happens, often by accident. The water temperature you use is very important. Hot water strips away natural oils like butter melts under heat.
Always use lukewarm water instead of hot. Hot water dissolves the fatty layer that protects your skin, making it weak and open to damage.
Choose soap-free cleansers made for sensitive skin. These clean well without harsh ingredients that harm the barrier. Look for pH-balanced and fragrance-free options to avoid irritation.
How often and how long you cleanse also affects skin barrier repair. Cleansing too much removes oils faster than your skin can replace them. Clean your skin once or twice a day, depending on your needs.
When you do cleanse, keep it short and focused:
- Massage cleanser onto skin for only 30-60 seconds maximum
- Use gentle circular motions instead of harsh scrubbing
- Avoid long massage that breaks down barrier lipids
- Rinse thoroughly but quickly with lukewarm water
- Pat skin dry with a soft towel instead of rubbing
The goal is to remove dirt, makeup, and excess oil without stripping away essential barrier components. Think of cleansing as maintenance, not deep scrubbing. Your skin needs its natural oils to work right.
Moisturizing Ingredients to Look For
Effective skin barrier repair means replacing what’s missing for your barrier to rebuild. Not all moisturizers are the same. Knowing which ingredients help recovery helps you choose better.
Ceramides are the main ingredient to look for in barrier repair products. They fill gaps between skin cells, keeping moisture in. Without enough ceramides, your barrier can’t stay strong.
Your repair routine should include products with these barrier-supportive ingredients:
- Fatty acids like linoleic and linolenic acids provide essential building blocks
- Cholesterol works with ceramides to strengthen the barrier structure
- Hyaluronic acid attracts and binds water molecules in your skin
- Niacinamide boosts natural ceramide production
- Glycerin draws moisture from the environment
- Squalane reinforces lipid structure and prevents water loss
Knowing the difference between humectants and occlusives is key for full barrier recovery. Humectants like hyaluronic acid and glycerin draw water into your skin. Occlusives and emollients like ceramides and squalane seal that moisture in.
You need both types working together for the best skin barrier repair. Using only humectants can pull moisture out of deeper skin layers if not sealed. Layering products correctly creates the best healing environment.
Start by checking your current products’ ingredient lists. Replace items lacking barrier-supportive components with formulas made for sensitive skin. Every product in your routine should add moisturizing benefits, not just extra steps.
Consider building a simple but effective routine for repair. Use a gentle cleanser, followed by a ceramide-rich serum, and a moisturizer with multiple barrier lipids. Adding a product with hyaluronic acid between cleansing and moisturizing helps keep hydration in.
Remember, barrier repair takes time and consistency. You won’t see quick changes, but with these practices, your skin will slowly get its protective function back. Stick with gentle methods and supportive ingredients for lasting results.
Products to Support Skin Barrier Health
Choosing the right products for your skin barrier is key. It’s not just about picking anything. You need to know which ingredients really help your skin recover. The market is full of products claiming to fix your barrier, but some ingredients are backed by science.
Good products for your barrier do more than one thing. They give your skin what it needs to fix itself and keep it moist. This helps fix the gaps in your barrier and stops moisture loss.
Ceramide-Rich Formulations for Barrier Restoration
Ceramides are essential for fixing your barrier. They make up about half of your skin’s natural lipids. When your barrier gets damaged, ceramide levels drop, leaving gaps. Products with ceramides help fill these gaps by giving your skin what it needs to repair itself.
There are many types of products that work well. Gentle cleansers with ceramides clean your skin without stripping it. They also include oils that help keep your skin healthy while removing dirt.
Ceramide serums are another great option. They are lightweight and get deep into your skin. Use them before moisturizer to help fix your barrier.
Look for moisturizers that have ceramides and other lipids. These products have fatty acids, cholesterol, and natural oils. They help fix your barrier better.
- Fatty acids strengthen cellular bonds
- Cholesterol fills spaces between cells
- Natural oils mimic your skin’s natural makeup
- Peptides signal your skin to repair itself
Barrier repair creams have ceramides in the right amounts. This helps them work better. Using them regularly helps your barrier get stronger over time.
Ceramides fill gaps in your skin’s structure. As they work, they help your skin hold water and protect itself. This makes your skin less sensitive, dry, and inflamed.
Hyaluronic Acid’s Hydration Support
Hyaluronic acid is important for keeping your skin moist. It can hold a lot of water, pulling it into your skin. While it doesn’t fix lipids, it helps your skin recover by keeping it hydrated.
Your skin can’t fix itself if it’s dry. It needs water to repair and make new lipids. Hyaluronic acid keeps your skin hydrated, helping it repair itself.
The size of hyaluronic acid matters. Products with different sizes work best:
- Big molecules form a moisture film
- Medium molecules get into the top layers
- Small molecules get deep into your skin
To get the most out of hyaluronic acid, use it right. Apply it to damp skin, then put on a moisturizer to keep the moisture in. Without a moisturizer, it can pull moisture out of your skin, making it drier.
Using hyaluronic acid with niacinamide is even better. Niacinamide helps your barrier by making more ceramides and reducing inflammation. Together, they help your skin stay hydrated and fix itself over time.
A good routine includes a gentle cleanser, a hyaluronic acid or niacinamide serum, and a ceramide moisturizer. Finish with squalane oil. This combination helps your skin in many ways, speeding up recovery and preventing damage.
Seeking Professional Help
At times, the best thing for your skin is knowing when to seek professional help. While good skincare routines help many, some issues need a dermatologist’s expertise. Getting expert care is a smart choice that leads to better results.
Knowing when to stop self-care protects you from more harm. If your skin doesn’t get better with home care, see a doctor. Dermatologists can find and fix problems you can’t see.
Recognizing When Medical Evaluation Becomes Necessary
Some signs mean you need a dermatologist. If your skin doesn’t get better after 4 to 6 weeks of care, it’s time to see a doctor. You should see some improvement in this time.
Severe symptoms need immediate attention. This includes widespread inflammation, oozing skin, and pain that stops you from doing daily tasks. Also, sudden changes without a clear reason should be checked by a doctor.
Recurring problems need a specialist’s help. If you keep facing the same skin issues, a dermatologist can find the cause. Conditions like adult acne and eczema often affect the skin barrier.
Seek help if you’re worried or unsure about your skincare. Dermatologists can guide you through the many skincare options. They help you find the right products for your skin, including pH balance.
If you have a damaged skin barrier due to an underlying skin condition, you should work with a dermatologist to ensure you’re doing what’s right for your specific needs.
Available Treatment Options and Consultation Methods
Seeing a dermatologist offers more than home care. They will examine your skin and review your medical history. This helps them understand what’s causing your skin problems.
Dermatologists might suggest tests to find allergies or confirm conditions. Patch tests and skin biopsies are examples. These tests help find the right treatment.
Prescription treatments can work better than over-the-counter products. Topical corticosteroids reduce inflammation fast. Prescription creams help repair the skin barrier. Medications for conditions like eczema need a doctor’s guidance.
Professional treatments help restore your skin barrier. Chemical peels and LED therapy are examples. These treatments work with your home care routine.
There are many ways to see a dermatologist today. You can visit in person or use teledermatology for convenience. Both options connect you with experts.
Choose board-certified dermatologists for treatment. They have the training to diagnose and treat your skin problems correctly. They use the latest research to help your skin.
This article is for education, not medical advice. Everyone’s skin is different, needing unique care. Professional help ensures you get the best treatment for your skin.
Conclusion: Protecting Your Skin Barrier
Knowing the signs of barrier damage lets you act fast. This knowledge helps you spot issues with your skin’s protection. Remember, everyone’s skin reacts differently to products and treatments.
Daily Care Practices
Keeping your barrier healthy needs ongoing effort. You can’t just fix it once and forget. The healing process takes three to four months to see real changes.
Healing dry skin takes time, just like restoring your barrier. Keep using moisturizing products even after your skin looks better. Always use broad-spectrum SPF 30 or higher sunscreen daily. Sun exposure can cause long-term damage.
Avoid harsh treatments and don’t overdo it with active ingredients like acids or retinol. They can undo your progress fast.
Adjusting to Life Changes
Your skincare routine should change with the seasons and life stages. Use richer moisturizers in winter and lighter ones in summer. Watch for signs like tightness or redness in your skin.
This article aims to educate you about your skin. It’s not meant to diagnose or replace a dermatologist’s advice. Skin issues vary greatly among people. Always talk to a professional for serious or ongoing problems.


