Up to 65% of people with darker skin get dark spots after acne or irritation. Yet, many think these spots are new breakouts. This guide helps you spot PIH early, so you can treat it before it gets worse.
PIH looks like flat tan, brown, dark brown, or blue-gray patches. They stay after a pimple, rash, cut, or procedure heals. In bright light, their edges are sharp and smooth, unlike active acne. Sun makes these spots darker, so always use sunscreen, even on cloudy days.
This guide teaches you to spot PIH by sight and pattern, not guesswork. You’ll learn how these spots form, who’s at risk, and when to see a dermatologist. It’s all about clarity: simple checks at home to tell PIH from scarring or new inflammation.
If you see spots that match your recent skin event, like acne or a scratch, watch their color, shape, and how they change with light. These signs help confirm PIH and guide better care choices.
Key Takeaways
- PIH shows as flat tan to dark-brown or blue-gray spots that remain after inflammation fades.
- Color often deepens with sun, making daily SPF a core step in United States skincare.
- Match the spot’s location to a recent trigger—acne, eczema, irritation, or minor injury.
- Edges are usually smooth and well defined, unlike raised or tender active lesions.
- Epidermal PIH tends to fade in months; deeper hues may persist longer without care.
- Recognizing PIH early helps you avoid harsh scrubs and choose proven treatments.
- If spots spread, change fast, or look unusual, seek a dermatology evaluation.
What is Post-Inflammatory Hyperpigmentation?
Post-inflammatory marks can seem hard to get rid of, but they follow a clear pattern. Knowing what Post-Inflammatory Hyperpigmentation (PIH) is helps set realistic goals and supports smart prevention. In dermatology, the focus is on why color changes linger after irritation and how to lower future risk.
Definition and Overview
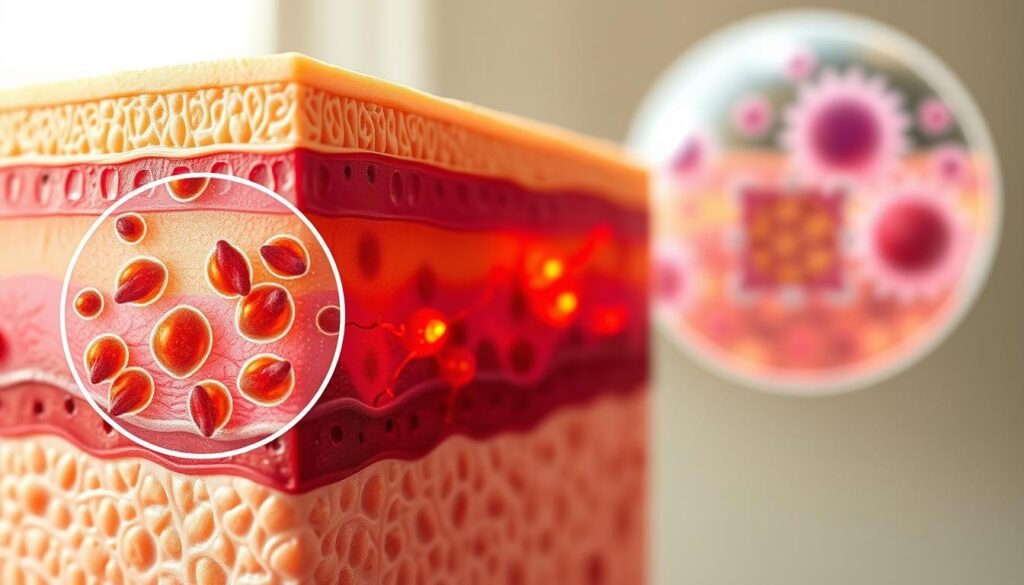
At its core, Post-Inflammatory Hyperpigmentation refers to extra pigment that appears after the skin is inflamed or injured. It shows up as tan, brown, dark brown, or blue-gray spots and patches. These changes are common in post-inflammatory skin conditions and can involve the surface or deeper layers.
During a flare, chemical signals spark melanocytes to make more melanin. This overproduction and uneven spread lead to visible discoloration. In dermatology PIH, epidermal color tends to look brown, while deeper dermal pigment can look blue-gray.
People with darker skin tones often notice more intense and longer-lasting marks. Consistent sun care and gentle routines form the base of PIH prevention and help improve tone over time.
Causes and Triggers
Common hyperpigmentation causes include acne, eczema, and minor trauma like scratches or burns. Shaving that leads to razor bumps, friction from tight gear, and picking at lesions make spots worse. These triggers are frequent in post-inflammatory skin conditions across ages.
Infections, psoriasis, and allergic rashes can spark new patches. Dermatology PIH may also follow procedures that inflame the skin, such as chemical peels, laser treatments, cryotherapy, or radiation therapy. Summer UV exposure darkens existing marks and extends how long they stay.
Reducing irritation, using non-comedogenic products from brands like CeraVe, La Roche-Posay, and Neutrogena, and daily broad-spectrum SPF support PIH prevention. These steps limit new flares and help fade current discoloration.
| Trigger | Typical Appearance | Layer Most Affected | Helpful Habit for PIH Prevention |
|---|---|---|---|
| Acne and picking | Tan to brown spots after lesions heal | Epidermis | Hands off lesions; use benzoyl peroxide or adapalene as directed |
| Eczema flare | Patchy brown areas post-itch | Epidermis and superficial dermis | Moisturize twice daily; avoid harsh soaps |
| Razor bumps (pseudofolliculitis) | Dark spots on beard, neck, or bikini line | Epidermis | Use sharp single-blade or electric trimmer; shave with the grain |
| Procedures (laser, peels, cryotherapy) | Diffuse darkening in treated zones | Dermis and epidermis | Pre- and post-procedure sun protection; follow aftercare |
| UV exposure | Worsening depth of color in summer | Epidermis | Daily broad-spectrum SPF 30+; reapply every 2 hours outdoors |
Symptoms and Visual Characteristics
Post-inflammatory marks show up where the skin healed from a flare, nick, or bite. PIH recognition starts with noticing timing. Patches appear after swelling or irritation fades.
These areas are flat, not raised, and show visible skin discoloration. This discoloration can last for months.
Color Variations
Shallow changes often look tan, brown, or dark brown. These dark spots on skin may brighten over time. This happens with consistent sun protection and gentle care.
Many people notice color changes after acne along the jawline or cheeks. This is where breakouts were most active.
Deeper marks can shift to a blue-gray cast. This pattern hints at pigment sitting lower in the skin. It’s a hallmark seen in stubborn pigmentation disorders.
Such tones tend to last longer. They may resist routine brightening products.
Common Skin Areas Affected
Spots arise where the trigger occurred. On the face, past acne, eczema, or ingrown hairs can leave skin discoloration. The neck and forearms, which get frequent sun, show seasonal darkening.
This makes PIH recognition easier.
On the trunk and limbs, scratches, rashes, bug bites, and minor burns can leave dark spots on skin. Beard zones prone to razor bumps often display color changes after acne and shaving irritation.
This contributes to visible pigmentation disorders in daily light.
Risk Factors for Developing Hyperpigmentation
Some spots just won’t go away. Experts say it’s because of many reasons, from our biology to our daily habits. In the United States, protecting our skin from the sun is key. This is because sun exposure can make spots darker after even a small injury.
Skin Types and Genetic Predisposition
People with more melanin are at higher risk for hyperpigmentation after injuries. Studies show that darker skin types are more likely to have deeper and more frequent spots. This is true for many people of African, Asian, and Latin American descent.
Age and gender don’t really affect the risk. But, if you have a family history of dark spots, you might be more likely to get them. When you have acne or eczema, you might notice darker spots that last longer. Looking at guidance on dark spots can help you understand and prevent them.
Environmental Influences
UV radiation is a big environmental trigger. In the summer, when the sun is strongest in the United States, spots can darken. Heat, sweat, and friction from masks or collars can also cause stress. Shaving or ingrown hairs can irritate hair follicles and lead to more spots.
Using strong peels or the wrong laser settings can increase the risk of hyperpigmentation, too. Insect bites, harsh scrubs, and picking at acne can also make spots worse. Using sunscreen, shaving carefully, and taking care of your skin can help prevent lasting spots.
| Factor | Mechanism | Higher-Risk Profiles | Practical Tip |
|---|---|---|---|
| Fitzpatrick Skin Type | More reactive melanocytes increase pigment after inflammation | Types IV–VI; African, Asian, Latin American descent | Patch test actives; favor gentle, non-irritating routines |
| UV and Heat | UV drives melanogenesis; heat and sweat prolong redness | Outdoor workers; high-UV regions and summer months | Broad-spectrum SPF, hats, shade; cool skin post-exercise |
| Friction and Grooming | Microtrauma from masks, collars, or shaving sparks PIH | Curly/coily hair prone to razor bumps; tight clothing | Use lubricating shave gels; reduce rubbing; switch fabrics |
| Procedures and Products | Harsh peels or unsuitable lasers trigger inflammation | Darker tones; recent tanning | Seek providers experienced with skin of color; gradual treatments |
| Picking and Scratching | Prolonged injury deepens and extends pigmentation | Acne, eczema, or bug bites | Hands-off approach; spot patches; anti-itch care |
Mechanism of Hyperpigmentation Formation
Inflamed skin starts a chain reaction that leads to dark marks after acne, eczema, or a rash. Knowing how PIH works helps us understand where and for how long these marks stay. Dermatologists look at the depth, cause, and signals that make melanocytes produce more pigment.
How Inflammation Leads to Dark Spots
When skin gets hurt, inflammatory substances rush in. Cytokines, prostaglandins, and reactive oxygen species wake up melanocytes and mess with their communication with keratinocytes. This mess leads to more melanin being made at the injury site.
In epidermal vs dermal PIH, where the pigment settles matters. In the top layer, extra pigment shows up as brown spots. If it gets into the deeper layer, it turns blue-gray and lasts longer.
Looking at skin samples shows how this works. In the top layer, melanocytes are active but intact. In the deeper layer, cells filled with pigment are seen. Sunlight makes things worse by boosting inflammation and oxidative stress.
Role of Melanin Production
After inflammation, melanin production goes up, thanks to tyrosinase. People with darker skin tend to have more active melanocytes. This makes the pigment response stronger and longer-lasting, a key part of PIH.
How deep the pigment is affects how long it lasts. Top layer pigment fades as skin cells turn over. But deeper pigment takes longer to go away because it’s held by cells in the deeper layer.
Ultraviolet light also makes melanin production go up. Wearing broad-spectrum sunscreen every day helps control inflammation and prevent new or darker spots.
Conditions Associated with Post-Inflammatory Hyperpigmentation
Many skin conditions leave dark marks after they heal. These marks happen when inflammation messes with melanin balance. This is a common issue in dermatology PIH. Things like seasonal changes, scratching, and irritation can make these marks more noticeable on all skin tones.
Understanding the trigger helps shape prevention and aftercare. Acne is a big cause of hyperpigmentation, but other issues like rashes and injuries can also lead to dark spots. It’s important to reduce friction, stop picking, and control inflammation early.
Acne and Inflammatory Skin Conditions
Acne papules, pustules, and nodules often lead to hyperpigmentation. After a breakout heals, brown to gray macules may stay, mainly where lesions were deep or picked. Shaving bumps and bacterial infections like impetigo can also cause spots.
Other conditions like lichen planus, pityriasis rosea, lichen simplex chronicus, and papulosquamous eruptions can also lead to PIH. These conditions often happen due to friction, scratching, or irritation from clothing and grooming tools.
- Limit picking and squeezing to reduce pigment spread.
- Use gentle razors or guarded trimmers to curb follicular irritation.
- Control flares early with evidence-based care guided by a clinician.
Eczema and Psoriasis
Atopic dermatitis flares often leave flat macules known as eczema-induced PIH. Scratching makes these marks worse and can slow healing. Contact dermatitis and insect bites can also cause similar marks after redness fades.
Psoriasis plaques can leave psoriasis pigmentation changes, mainly after irritation or when scales lift. Winter dryness and summer heat or sweat can make these marks more visible, making PIH more noticeable during seasonal swings.
| Trigger | Typical Lesion | PIH Pattern | Aggravating Factors | Supportive Care Focus |
|---|---|---|---|---|
| Acne vulgaris | Papules, pustules, nodules | Acne-related hyperpigmentation on face, jawline, back | Picking, friction from masks or helmets | Breakout control, hands-off approach, non-comedogenic care |
| Pseudofolliculitis barbae | Shaving bumps and ingrown hairs | Brown macules and scarring along beard or neck | Close shaving, multi-blade razors | Guarded trimming, single-blade technique, soothing aftercare |
| Impetigo | Crusted bacterial lesions | Residual spots after crusts resolve | Delayed treatment, scratching | Prompt antibacterial therapy, wound hygiene |
| Atopic dermatitis | Pruritic eczematous patches | Eczema-induced PIH at sites of healing | Scratching, dry air, harsh soaps | Moisturizers, itch control, gentle cleansers |
| Psoriasis | Well-defined plaques with scale | Psoriasis pigmentation changes post-flare | Irritation, friction, seasonal swings | Plaque control, emollients, minimize trauma |
| Contact dermatitis | Red, itchy rash from exposure | Localized PIH in contact zones | Repeat exposure, occlusion | Allergen avoidance, barrier repair |
| Insect bites | Pruritic papules | Discrete spots where bites healed | Scratching, heat, sweat | Anti-itch care, bite prevention |
| Dermatologic procedures | Laser, light, peels, cryotherapy | Procedure-related dermatology PIH | Sun exposure, aggressive settings | Pre/post-care plans, strict photoprotection |
Diagnosis of Post-Inflammatory Hyperpigmentation
Getting a clear story is key to diagnosing PIH. It’s about where the spot started, what injury or inflammation came first, and how the color changed over time. A careful look at the location, borders, and shade helps match the lesion with a known trigger. This approach helps avoid unnecessary treatments.
Clinical Evaluation
The exam looks at spots or patches where acne, eczema, or friction happened. A Wood lamp test helps tell if the pigment is in the top layer of skin or deeper. This helps plan the treatment.
If it’s hard to tell what’s causing the spot, a biopsy might be needed. It can show if there’s more melanin in the skin or if there are melanophages. In some cases, blood tests can help find other conditions like Addison disease or lupus.
During the visit, the doctor will note the timing, sun exposure, and any products used. This careful evaluation helps make a confident diagnosis without overtesting.
Importance of Differentiation from Other Conditions
It’s important to rule out other conditions to avoid making things worse. Melasma is often caused by hormonal changes and shows up symmetrically on the face. It gets darker with UV exposure.
Other conditions that look similar include solar lentigines, tinea versicolor, and more. Knowing the difference helps choose the right treatment and protect the skin.
| Feature | Post-Inflammatory Hyperpigmentation | Melasma | Solar Lentigines | Tinea Versicolor |
|---|---|---|---|---|
| Typical Trigger | Inflammation or injury at same site | Hormonal influence; UV exposure | Chronic sun exposure | Malassezia yeast overgrowth |
| Distribution | Matches prior lesion pattern | Symmetric facial patches | Dorsal hands, face, shoulders | Trunk; patches may coalesce |
| Wood Lamp | Epidermal: accentuation; Dermal: none | Often epidermal accentuation | May accentuate lightly | Variable; may show contrast |
| Symptoms | Asymptomatic discoloration | Asymptomatic | Asymptomatic | Mild itch; scale possible |
| Key Clue | History of acne, eczema, procedures | Pregnancy, oral contraceptives | Photoaging signs present | KOH can reveal hyphae |
| Management Impact | Target pigment depth; protect barrier | Hormonal and UV control essential | Photoprotection; pigment modulators | Antifungal therapy first-line |
By combining PIH diagnosis with a careful look at other conditions, doctors can choose the right treatment. This approach improves results and helps refine the assessment of pigmentation disorders.
Treatment Options Available
Effective PIH treatment starts with calming the original flare, whether acne or eczema. Results build slowly, and steady routines matter. Sun defense underpins every plan and keeps gains from fading.
Topical Treatments
Most patients do best with a combined approach. A proven trio uses hydroquinone 4%, tretinoin 0.05%, and fluocinolone acetonide 0.01% for a limited steroid window. This mix targets pigment, boosts turnover, and eases irritation.
When skin is sensitive, mequinol, azelaic acid, or stabilized cysteamine can be added or swapped. Retinoids for hyperpigmentation—tretinoin, adapalene, and tazarotene—also help clear acne that fuels dark marks. Expect months of use, with progress tied to daily sunscreen.
Chemical Peels and Laser Therapy
Carefully timed chemical peels such as glycolic acid, salicylic acid, or low-strength trichloroacetic acid lift pigment in the upper skin layers. An experienced clinician adjusts strength and spacing to limit irritation and rebound darkening.
For stubborn spots, laser therapy can help. Q-switched ruby and Q-switched Nd:YAG, picosecond devices, and fractional systems demand expert settings, even on deeper skin tones. Test spots, conservative energy, and strict aftercare reduce risk.
Preventive Measures
Daily broad-spectrum sunscreen and shade habits are key to PIH prevention. Treat breakouts early, avoid picking, and reduce friction from masks, hats, or tight collars. Choose gentle cleansers and non-comedogenic moisturizers that support barrier repair.
Plan for seasonal UV spikes with reapplication every two hours outdoors and UV-protective clothing. Clear timelines and realistic goals keep motivation high and protect the gains from each phase of PIH treatment.
Home Remedies for Post-Inflammatory Hyperpigmentation
Home care can help fade marks while protecting your skin. Start with simple steps to reduce irritation and keep moisture in. Adjust your routine based on how your skin reacts.

Natural Ingredients to Consider
Over-the-counter options can brighten your skin without harsh scrubbing. Azelaic acid helps even tone and calm redness. Low-dose glycolic acid offers gentle exfoliation that improves texture over time.
Niacinamide serums are great for supporting the skin barrier and reducing dullness. Choose fragrance-free formulas from brands like The Ordinary, La Roche-Posay, and CeraVe. Use them with a bland moisturizer to prevent dryness.
- Azelaic acid: Start a few nights per week and increase as tolerated.
- Glycolic acid (low strength): Use sparingly; avoid stacking with other acids.
- Niacinamide: Morning or night, works well with sunscreen for PIH prevention.
These options can be part of your home care routine with patience. Results may vary, and deeper spots might not fully respond to topical treatments.
Safety and Efficacy
Be careful with DIY treatments. Avoid strong peels, abrasive scrubs, or at-home devices that can irritate your skin. If you experience stinging, peeling, or redness, stop and seek advice.
Epidermal marks may fade in 6–12 months with consistent care. Deeper PIH can take much longer. Always use daily sunscreen with broad-spectrum SPF 30 and zinc oxide, and reapply when outdoors.
- Patch test new products for 24–48 hours before full use.
- Introduce one active at a time to judge tolerance.
- Moisturize after actives to maintain barrier health.
- Combine home care with professional advice for stubborn areas.
Balance natural brightening ingredients with caution. Sustainable routines reduce risk while supporting gradual progress for PIH and skin discoloration at home.
The Role of Sun Protection
Sunlight can make dark spots worse and slow down healing. Using sunscreen every day helps protect against hyperpigmentation. It’s also key for preventing PIH, even in the summer.
Importance of Sunscreen
UV and visible light can make marks darker and cause new ones. Sunscreen is essential because it lessens how long and how dark these spots can get.
Choose a sunscreen you’ll use often. Look for one with broad-spectrum protection and at least SPF 30. Make sure to apply enough to your face, ears, and neck. Reapply every 80 minutes outside, and more if you’re swimming or sweating.
- Look for zinc oxide near 8% for reliable coverage.
- Add shade, UPF clothing, and a wide-brim hat for an extra layer.
- Get vitamin D from diet or supplements instead of unprotected sun.
Choosing the Right SPF
When picking SPF, choose broad-spectrum protection that blocks UVA and UVB. Mineral options with zinc oxide or titanium dioxide are good for sensitive skin. They come in newer tints that don’t leave a white cast.
Water-resistant formulas are great for workouts or beach days. They help keep your skin protected all day. Use a nickel-sized amount on your face and two tablespoons on your body before going outside.
| Need | Recommended Features | Why It Helps | Examples of Options |
|---|---|---|---|
| Daily city wear | Broad-spectrum SPF 30+, lightweight finish | Shields from incidental UV that worsens dark spots on skin | La Roche-Posay Anthelios Melt-in Milk SPF 60; CeraVe Hydrating Mineral SPF 30 |
| Sensitive or acne-prone skin | Mineral filters (zinc oxide, titanium dioxide), non-comedogenic | Lower irritation supports sun protection for hyperpigmentation | EltaMD UV Clear SPF 46; Aveeno Positively Mineral Sensitive Skin SPF 50 |
| Outdoor sports and beach | Water-resistant 80 min, SPF 50+, sweat-resistant | Stable film helps prevent streaks and gaps during activity | Neutrogena Sheer Zinc SPF 50; Blue Lizard Sensitive Mineral SPF 50+ |
| Deeper skin tones | Tinted mineral or sheer chemical-mineral blends | Improved wear reduces cast while maintaining coverage | Unsun Mineral Tinted Face SPF 30; Black Girl Sunscreen Broad Spectrum SPF 30 |
Lifestyle Changes to Prevent Hyperpigmentation
Making small changes in your daily life can help prevent PIH and improve your skin. Eating right, using gentle skincare, and protecting your skin from the sun are key. These steps can help reduce dark spots and improve your skin’s color over time.
Diet and Hydration
Eat lots of colorful fruits and veggies, lean proteins, and healthy fats. These foods help your skin stay strong and recover quickly. Drinking water all day keeps your skin moist and less likely to get irritated.
If you stay out of the sun to prevent PIH, get vitamin D from food or supplements. Salmon, fortified milk, and eggs are good sources. Drinking water and eating well also helps by keeping your skin from getting dry and itchy.
Skincare Routine Adjustments
Make a skincare plan that avoids rubbing and picking. Use soft clothes, change masks often, and treat acne or eczema early. Choose products that are fragrance-free and won’t clog pores.
Start with gentle ingredients like azelaic acid and retinoids. Brands like The Ordinary, La Roche-Posay, or Differin offer them. Use them a few nights a week and increase as your skin gets used to it. Avoid harsh scrubs and use chemical exfoliants as your dermatologist suggests.
Shave carefully to avoid razor bumps. Clean your skin first, use a gel from Gillette or Cremo, and change your blade often. Use richer moisturizers in winter and lighter ones in summer. Always apply broad-spectrum SPF 30 or higher in the morning to protect your skin.
When to Seek Professional Help
Knowing when to see a dermatologist can save you months of trying different things. If spots don’t go away or spread, it’s time to visit a dermatologist. A quick visit can help you understand what’s happening with your skin.
Signs That Require Medical Attention
Make an appointment if spots change color fast, spread a lot, or show up without a reason. Also, if new dark spots appear after inflammation, it’s urgent. Look for signs like fatigue, dizziness, or new rashes, which might need more than just skin care.
It’s smart to see a dermatologist if home treatments don’t work after a while. If you’re thinking about peels or lasers, it’s best to talk to a professional. These signs might mean your skin needs special care.
Importance of Dermatological Consultation
A dermatologist can give you a plan that fits your skin type and how deep the spots are. They might use a Wood lamp or take a biopsy. This helps find the right treatment for you.
Dermatologists can prescribe special creams and might suggest peels or lasers. They know how to choose treatments that are safe for darker skin. They also work with other doctors to make sure you get the best care.
They’ll tell you how long things will take, how to protect your skin from the sun, and how to track your progress. If you’re not sure when to see a dermatologist, wait until spots last more than a few months or get worse with home care.
Emotional and Psychological Impact
Post-inflammatory hyperpigmentation may not hurt, but it can affect your daily life. It can make you worry, pull you back from social events, or lower your mood. If spots last long, it can be really frustrating, affecting your life quality.
Knowing what to expect can help. Marks on the skin’s surface might fade in 6–12 months. But, deeper spots or in darker skin tones can last years or even be permanent.
Effects on Self-Esteem
When you have skin discoloration, it can affect how you feel about yourself. You might avoid photos, change what you wear, or skip out on events. If treatments don’t work or make things worse, it can be really tough.
Working with a dermatologist can help. They can create a plan that works for you. This can help you feel more confident again.
Strategies for Coping with Skin Concerns
There are simple ways to cope with skin issues. Use gentle cleansers and avoid rough scrubs. Choose products that are gentle and won’t irritate your skin.
Wearing sunscreen every day helps keep your skin tone even. It also prevents new spots from getting darker. This can help you feel better as you wait for your skin to improve.
For a quick boost, try makeup for PIH. Look for products that won’t clog pores and match your skin tone. Use peach or orange color correctors under your makeup to help even out your skin.
Don’t forget about your mental health while treating your skin. Talking to a counselor, joining a support group, or practicing mindfulness can help. Work with a dermatologist to find safe treatments and avoid making things worse.
Always talk to a healthcare professional before changing your skincare or routine. A careful plan protects your skin and well-being while you heal.


